Guidance about the role of speech and language therapy in working with augmentative and alternative communication (AAC) for SLTs
Last updated: May 2024
About this guidance
“An item on a communication aid is not just a word. It is a strategy to make another person infer a word.” (von Tetzchner et al, 2024)
This guidance aims to support RCSLT members to recognise, assess and offer intervention to people who may benefit from augmentative and alternative communication (AAC) tools, techniques or strategies. This will be achieved by using evidence-informed practice, which includes:
- appreciating the lived experience of the AAC user*, their families and support networks and the impact this may have on intervention decisions
- describing why an AAC user may have different communication support needs in varying contexts
- describing the things that impact on the efficiency of speech, language and communication
- describing the types of AAC tools, techniques and strategies that may enhance speech, language and communication
- describing the ways in which AAC may enable individuals to communicate effectively and how this differs from using spoken words.
It also aims to provide clarity about the role of the speech and language therapist (SLT) working with AAC users. This will include:
- consideration of direct management and intervention approaches
- working collaboratively with AAC users, family members, other professionals and stakeholders (such as those in the community and voluntary sectors)
- working collaboratively with other SLTs who share AAC knowledge and may work in the NHS, or independently, or those SLTs employed directly in a range of establishments, such as schools, colleges and care homes
- The role of SLTs in advising commissioners and policy makers
*Throughout this guidance we will use the term ‘AAC user’ to represent variations in the descriptive terms that may be used. As AAC is an intervention, rather than a diagnostic term, we will use identity-first language, i.e. ‘AAC user’. We acknowledge that existing literature uses terms such as ‘Person who uses AAC (PwuAAC)’, ‘Person with complex communication needs (CCN)’, or ‘aided communicator’. However, a poll initiated by Communication Matters determined that ‘AAC user’ was the preferred term in the UK. Individual choice of preferred term may vary and should be respected (see recent survey reinforcing this debate).
The guidance has been co-produced by those with lived experience and with SLTs from across the UK. It is acknowledged that many of the references and resources cited have not been co-produced.
This guidance takes a lifespan approach. We will use the words ‘people’ or ‘individuals’ when referring to all ages, only specifying ‘child’, ‘young person’ or ‘adult’ when a statement refers to a specific age group.
AAC in context – supporting diversity
This guidance focuses on an intervention. Augmentative and alternative communication (AAC) is a collective term summarising a range of tools, techniques and intervention approaches that may be used to enhance speech, language and/or communication. AAC may be used temporarily or be useful over someone’s lifetime as a main method of communication or a part-time method depending on the context and communication partners present.
The content within this guidance is written for speech and language therapists (SLTs). However, the field of AAC practice and research is collaborative and interdisciplinary; therefore, much of the content may be helpful to AAC users, family members and other professions or stakeholders.
The context of AAC practice and research is far ranging (Schlosser et al, 2005). It includes services to very young children or those with life-changing conditions that become evident during early childhood. It also includes services to support adolescents and adults with ongoing speech, language and communication challenges or difference. AAC also applies to those with acquired communication challenges or to those with progressive and life-limiting conditions. Changes in communication efficiency may be acquired in childhood, adolescence or adulthood. There are very few contexts of practice for SLTs where an AAC tool or technique is not relevant.
The aim of any AAC intervention is to support an individual’s autonomy and participation in everyday activities, whether they identify as neurotypical or neurodivergent (e.g. Walker, 2021). We recognise the linguistic and cultural perspectives of potential AAC users and their families (see Lynch and Murray, 2023; Sadiku et al, 2022; Tönsing and Dada, 2023). We adopt a user-centred, culturally sensitive approach to considering the available evidence for AAC interventions. An ecological validity framework enables consideration of human neurodiversity across multiple dimensions, including language, persons, concepts, goals and contexts (Perera et al, 2020; Bernal et al, 1995). Awareness of the diversity of potential AAC users informed our reviews of sources of evidence that may inform practice.
In reviewing the array of material, we consider types and levels of evidence. Knowing about levels of evidence helps us decide if we can make use of the information for an individual AAC user or family.
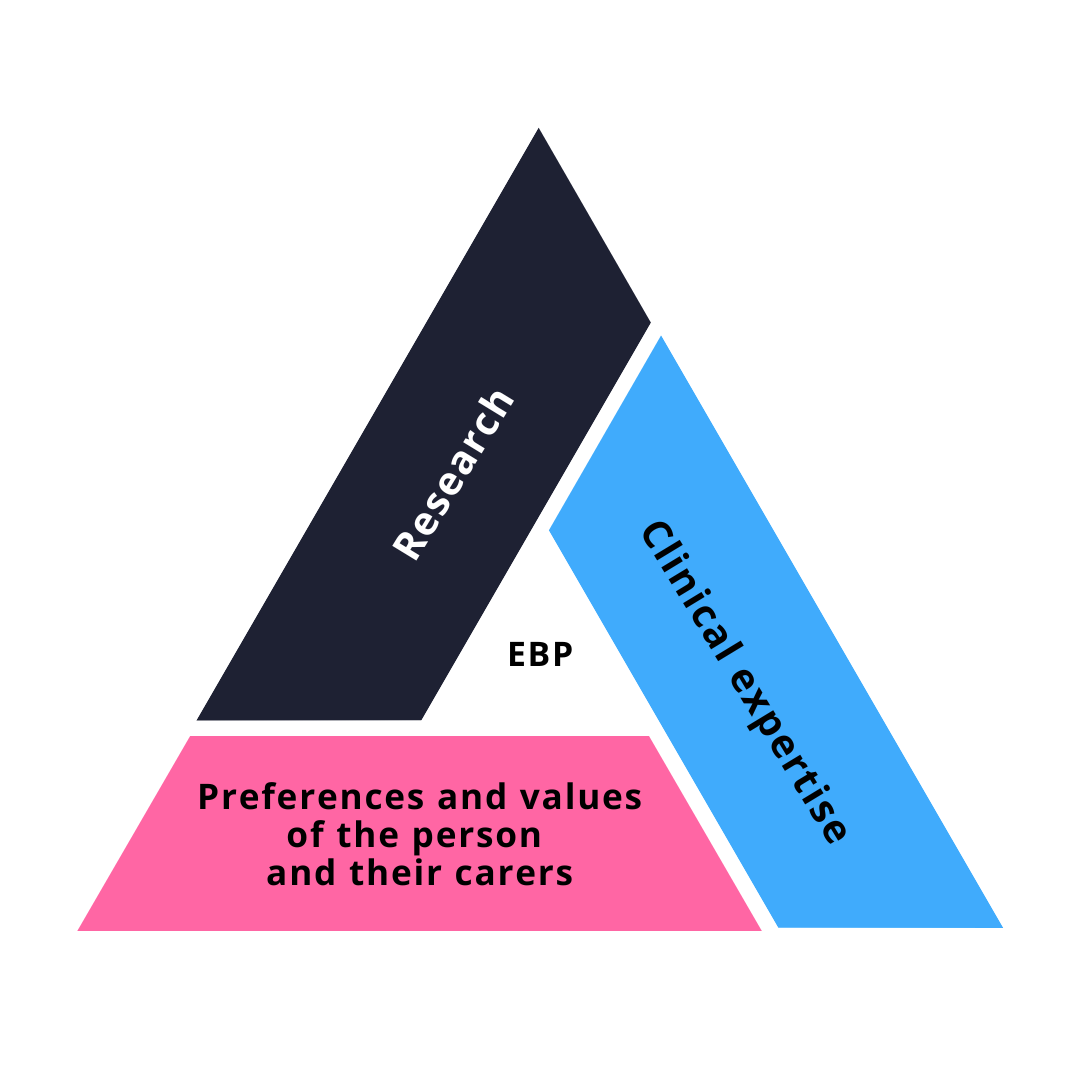
We consider three forms of evidence: research evidence, clinical practice evidence, and lived experience accounts. These comprise the RCSLT’s model of evidence based practice. This evidence can be found in scientific articles, general literature (journalism, blogs, magazines etc) or be practice based. These elements may influence the presenting characteristics of the individual who may use AAC, their environmental influencers and the activity and participatory enablers that an AAC intervention offers.
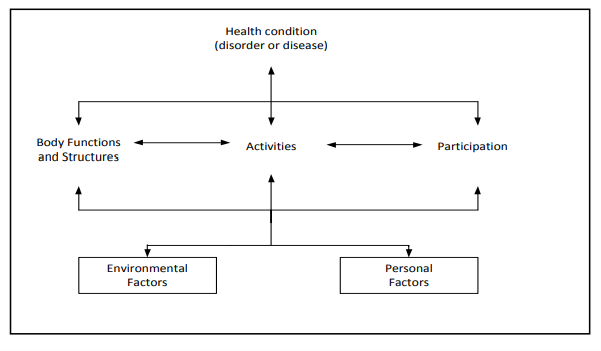
For the majority of potential AAC users, we can frame our considerations using the International Classification of Functioning, Disability and Health, as a bio-psycho-social model describing ability and potential, rather than inability (ICF, 2013; Raghavendra et al, 2007).
The ICF framework (PDF, external link) includes a figure (Figure 1 – also replicated below) which shows a schematic representation of the elements that may influence the presenting characteristics of the individual who may use AAC, their environmental influencers and the activity and participatory enablers that an AAC intervention offers.
Some cautionary notes:
- The array of available AAC tools, techniques and resources is extensive. It should not be assumed that one particular form of AAC is to be prized above all others. A ‘one system’ approach in any context may be problematic for individual AAC users. In fact, it is likely that more than one form of AAC is used regularly by an individual, e.g. key word signing plus a communication book.
- There are no pre-requisites to using AAC. However, many AAC systems may not be the most appropriate form of intervention for an individual at that point in time, or ever. Processes used in the identification of the relevant AAC tool/s vary depending on their contexts of use and the characteristics of each potential AAC user.
- Therapy using AAC to support speech intelligibility, language development, the ability to understand or communication efficiency is not the same as therapy supporting speech, language and communication where no AAC system is used.
- Introduction to, or provision of, an AAC resource is usually the beginning not the end of the intervention. We would not expect to become a proficient pianist by the mere provision of a piano. Therefore, we should not expect anything different in the introduction of an AAC system. Proficiency in any activity, including learning an AAC system may take 10,000 hours of effort. Much of this effort must be supported by SLTs and other key stakeholders (Omahen, 2009; Ericsson, Krampe and Tesch-Römer, 1993).
- Intervention provided over weeks or years to support AAC skill development is as important when considering unaided forms of communication, such as sign and gesture, as it is for aided systems, such as electronic devices.
- AAC intervention must be responsive to the multi-lingual aspects of society and the impact this will have on what AAC is available and needs to be developed to support equal access to communication resources.
- Whilst not ignoring unaided AAC, electronic developments are closely linked to aspects of assistive technology (AT), (e.g. environmental controls, educational technology) and artificial intelligence (AI) such as smart technology). In this guidance we remain focused on consideration of AAC, and, where relevant, highlight AI and AT components (g. Waller, 2019; Wang et al, 2023).
- It is important to note that appropriate AAC resource provision can happen via a local, specialist, independent or private service. Resource provision refers to people, time and type of AAC support. Current service and organisational structures vary across the four nations of the UK, including how these interact with each other. There may be lessons to share from these differences. For example, education, health and care plans (EHCP) or continuing health care (CHCP) plans mean something in England, but may not be known elsewhere. Also, the ‘hub and spoke’ model of specialised and local AAC provision is understood in England, Northern Ireland and Wales, but is not used in Scotland, where there are national, regional and local AAC services.
We reinforce the essence of the United Nations Convention on the Rights of People with Disabilities (CRPD, United Nations, 2006) as core values that influence all aspects of AAC intervention. Disability is a diverse and evolving concept and often results from the interaction between persons with perceived impairments and attitudinal and environmental barriers that hinder their full and effective participation in society on an equal basis with others. We must treat each person who may benefit from AAC as an autonomous individual who needs support in ways that enable their freedom of choice, independence and human interdependence that define all aspects of basic human rights.
AAC related terminology
What is AAC?
Augmentative and alternative communication (AAC) supports individuals to achieve their basic human right to be heard and included in an equitable way (Communication Matters, 2023).
AAC tools, devices, techniques and strategies may enhance speech, language and communication contributions for people who cannot entirely rely on their unsupported communication abilities to convey their intended message.
Communication challenges where AAC may be relevant may relate to physical, sensory, intellectual and neurodivergent perspectives, and learning or cognitive abilities. Applying the ICF model to explore the benefits of AAC enables us to consider the impact of body, structure and function or activity and participation characteristics (ICF, 2013). AAC users have unique needs that require AAC to be customised to meet their specific speech, language and communication abilities and challenges. An individual’s characteristics will change over time. An AAC method or tool must be chosen for how it can support communication changes. Use of AAC tends to result in a combination of several AAC strategies, rather than relying on, for example, one electronic communication device.
As communication includes more than just talking, AAC tools and techniques offer the user and their conversational partner/s different types of support:
- AAC can help an individual to understand what they might say and how they could say it. In this way the person can express thoughts and ideas when their unsupported speech, language or communication skills do not do justice to their desired contribution.
- AAC users (or anyone) rarely use just one communication method or tool. Synthesising use of more than one method of communication is critical to any intervention.
- AAC can support comprehension of contexts, conversational situations and enhance expressive skills.
- AAC may be used to support speech, language or communication development.
- AAC may act as a method for those with established speech, language and communication skills or support those losing these skills.
- AAC may support people to express their sense of identity, build social connections, relationships and realise aspects of self-determination that their communication otherwise restricts.
- The introduction of AAC requires communication partner training to ensure that individual AAC user abilities and needs are recognised and supported appropriately (see sections on ‘communication partners and types of AAC’ and ‘conversation partner training and support’).
- AAC users have differing abilities and bespoke communication support needs. It is important to find out what the AAC user wants. For example, some may require continual co-construction support and modelling, others do not require repeated modelling of messages.
Please note: to support longevity of this guidance we have avoided using the names of currently available products. Instead, we describe the principles and attributes each method of AAC offers. In this way readers will be able to describe what type of AAC system best supports the AAC user and apply that to currently available products.
Some AAC definitions
AAC strategies include both unaided and aided methods of communication. One challenge in the field of AAC is the array of terminology that may be used synonymously. The glossary provides explanations.
- Unaided communication refers to the use of methods involving the user’s body, such as body movements, facial expressions, gestures, key word signing, sign languages, eye-pointing, fixed gaze and vocalisations. One form of unaided communication includes a familiar person ‘re-voicing’ the AAC user’s own speech (Friedman et al, 2016, Pilesjö and Norén, 2019). Even with compromised physical abilities, unaided methods of communication can be quick and effective for many AAC users.
- Aided communication involves the use of physical tools and techniques. These can include paper-based materials as well as electronic devices. Aided communication methods are rarely as quick as an unaided method, but for many may offer more communication autonomy.
Both unaided and aided communication may include a level of co-construction of meaning between AAC users and conversational or communication partners (Smith, 2015).
Unaided suggestions:
Focusing on a person’s communication intentions as conveyed via body language, facial expressions, vocalisations, key word signing and sign language as ways to consider and understand communication intent.
Table 1: Summary of types of unaided AAC
| Unaided AAC (Many types listed are often used in combination by the AAC user) |
|
|---|---|
| Non-verbal (non-linguistic)* (note: these unaided methods are also used by non-AAC users, but AAC users may use them more often/as a predominant communication method) |
Verbal (linguistic elements) |
| Vocalisations (e.g. intonation-sounds, laughter, crying) | Signed vocabulary (e.g. Makaton) |
| Facial expressions | Sign supported English (or other non-English languages) |
| Body movements and gestures (e.g. tensing or arching of the back, turning head away, moving head upwards/downwards, pushing away, grasping something or someone, pointing) | Sign language (e.g. British Sign Language, Indian Sign Language) |
| Eye movements/gaze fixation (e.g. non-specific looking behaviour) | Eye-movement signals (e.g. yes = look up, no = look down) |
*There may be some specific meaning intended, but most signals conveyed are dependent upon the communication partner’s linguistic abilities or knowledge of the AAC user to interpret potential meaning.
Aided, non-powered suggestions:
Communication charts or boards, and notebooks or folders with no electrical power supporting their use. Vocabulary provided in these paper-based systems can be as extensive and as complex as many electronic systems. These non-powered solutions may use different types of communication referent, including real objects, or word, picture or symbol-graphic materials that act as conversational scaffolds (Harding et al, 2011).
Aided, powered suggestions:
Technology that makes use of equipment that has a power system. The device usually allows the individual to electronically access speech, picture, symbol-graphic, and/or written output.
There are a variety of powered systems. Some are dedicated communication aids; others use PC platforms or tablet devices. Each with different attributes, including different voices, shapes, sizes and weights, with capacity to store different amounts of vocabulary. This is done using a range of organisational structures, software packages, processing and internet platforms (Judge et al, 2023; Murray et al, 2019).
Table 2: Summary of types of aided AAC
| Attributes of aided AAC | |
|---|---|
| Paper-based | Powered |
| Representation of a word or concept (alphabet charts/written words/pictures/symbol-graphics/photos/real objects) | |
| Paper/cardboard/notebook/
Ring folder/plastic board/mat etc |
Device – box (dedicated aid, tablet, PC etc.)
|
| Battery or mains source/charging | |
| Software package/s for production and organisation of vocabulary | Software package/s for vocabulary organisation
Other software packages, e.g. cameras, stories, facilities for voice or message banking and apps |
| Operational software or platform | |
| Customisable sizes and weights | Differing weights and sizes |
| Can be attached or fixed with readily available solutions, e.g. hook-loop touch fastening | Mounting systems available, e.g. to attach to wheelchair or table |
| Co-produced speech/voice output with communication partner | Speech/voice output (including access to prestored voice and message banking facilities) |
| May include a message construction strip – if picture-graphics can be detached and moved | May include on-screen summary of message construction |
Accessing AAC
Accessing aided AAC
There are a range of ways to access an AAC system when direct access is difficult and individualised solutions may be required. Solutions to access needs may be bespoke, involving multidisciplinary professionals. As a minimum we would expect local and specialised services to include involvement of an occupational therapist, physiotherapist and rehabilitation engineer (or an equivalent term in regional locations) at some point. For example, while some people will use their fingers to point to part of a page or a screen (direct access), others who have additional physical challenges may benefit from accessing their AAC in different ways (indirect access). Alternative access features supporting aided communication could include non-powered and powered techniques.
Paper-based or non-powered access features could include eye-pointing, partner assisted scanning (where the partner acts as the ‘pointing finger’), auditory scanning (where the partner supports the AAC user with a visual impairment to hear what comes next) and use of vocalisation or gesture.
See:
- Partner assisted scanning (Ace Centre)
Accessing paper-based and powered AAC
Eye-pointing may involve unaided and aided techniques. For example, unaided techniques may involve looking at a desired object or person to convey a desire to have the object or to speak with the person. Aided techniques may involve paper-based or unpowered scaffolds, e.g. an Eye-Transfer frame (E-Tran frame), which is a clear perspex frame with visual referents attached. The communication partners are either side of the frame and use it as a means of recognising the eye-pointing choices of the AAC user while a message is constructed. Powered AAC alternatives are similar but include gaze-calibration of powered devices. Here, the individual uses gaze to indicate a direct choice of an item. In this way, eye-pointing offers direct access to a vocabulary item.
See:
- The new Ace Centre E-Tran Frame (Ace Centre)
- Rosemary: chatting with a Frenchay E-tran frame (Ace Centre)
Partner assisted and auditory scanning are both manual scanning methods supported by the communication partner operating as the pointer (by physically pointing to items and/or or reading them out loud). The AAC user can indicate a yes/no response to the options offered. This describes an indirect method of access to an item of vocabulary. Over time, using either approach allows the AAC user to build their desired message. Indirect scanning methods are not limited to these examples and may include encoded scanning, row column scanning and various alternatives. All these suggested access methods offer a tailored approach best suited to individual abilities and needs.

An eye-pointing access method, using a clear Perspex frame (image used with permission from Communication Matters)
Powered access features include anything that uses electricity and may be integral to the AAC system or standalone plug-ins, such as a switch, joystick, head mouse, touch screen or eye gaze unit and/or camera.
Switches offer indirect access to the vocabulary item, where an electronic scanning action is required. Joysticks or roller balls offer control of an on-screen cursor (similar to using a computer mouse). A touch screen, a head mouse or eye-gaze camera offers direct access to the vocabulary item. The principles of access are the same irrespective of paper-based/non-powered or powered methods.
See:
- Switch Scanning (North Bristol NHS Trust)
- Three Ways to Communicate With Me (head mouse use) (BBC Scotland)
Access features will require additional mounting and positioning technologies. Accurate positioning will involve a range of other professionals, including occupational therapist, rehabilitation engineer or healthcare scientist. Many of these services will be available locally, but for some these will only be available through UK specialised AAC provision (see Communication Matters). Services with an access focus may differ from those with an AAC and communication focus. This difference may cause some regional challenges in terms of how to refer, who to refer to and system/service expectations. This guidance cannot solve regional difference, but can highlight that there are differences. These differences may need higher level debate to resolve them.
Vocabulary considerations
The following considerations are most relevant to those using text based, picture and symbol-graphic representations of vocabulary. Unaided considerations of vocabulary choices for children are extensively considered by Grove and Launonen (2019).
Static, dynamic and visual scene displays
Communication boards and electronic communication systems can have static displays where all letter or vocabulary items are always on display, similar to a QWERTY keyboard on a laptop. However, communication books and electronic systems can also have dynamic displays. These allow the person to navigate to items by moving across levels or pages, similar to smart phone or laptop screens. These different ways of navigating to vocabulary place altered demands on learning and memory. These differing demands need to be considered when opting for one over the other (Thistle and Wilkinson, 2013). Consequently, SLTs need to explore memory, attention, sequencing and system navigation skills as a comprehensive aspect of determining which type of display may best suit the person now and in the future.
Powered visual scene displays provide a context for the user by having a photograph, picture or a virtual image. Behind the image there are ‘hot spots’ of stored messages or words. For example, a picture of a playground may include a girl on a swing. The swing has a ‘hot spot’ that when accessed says aloud ,‘whoop, I am up high’ and acts to reinforce a label, action or activity relevant to the visual scene (Beukelman et al, 2015; Thistle and Wilkinson, 2015). Visual scene displays are used most with emerging communicators, but also with those who have lost or are losing communication and cognitive skills (Dada et al, 2021; Dietz et al, 2006; Light et al, 2019).
Vocabulary organisation
Irrespective of the type of display used there are other considerations. Here, we consider how vocabulary is organised. This can be for individual paper pages (screens) or across a whole communication system.
It is worth noting that we do not speak a word by having it activated through the same neural route each time we use it. The domain of linguistics suggests the trigger for vocabulary access is context specific (Stadskleiv et al, 2022). There are potentially multiple routes to word retrieval. In AAC systems, vocabulary is typically organised in a row-column grid format for all forms of organisation, other than visual scene displays.
The three common forms of vocabulary organisation on AAC systems are: (i) taxonomic, (ii) semantic/schematic, and (iii) encoded (Beukelman and Mirenda, 2013).
(i) Taxonomic organisation: vocabulary is organised in categories, such as nouns, verbs, or topics (e.g. a list of clothing, transport, leisure pastimes). This allows an individual to give ‘key word’ information by accessing one page, but requires the AAC user to navigate multiple pages to build a sentence.
(ii) Semantic/schematic organisation: vocabulary is organised in such a way that a whole message can be produced from viewing and accessing one page. This will result in multiple appearances of the same vocabulary item across the whole AAC system, e.g. the verb ‘to go’ appears on several pages.
These organisational approaches include concepts of core/fringe vocabulary (Goossens’, 1994) and pragmatic organisation of words and symbols over several pages accessed in a dynamic manner (e.g. Porter and Cafiero, 2009).
(iii) Encoded (language) organisation: this involves sequencing two or more picture symbols, or logical letter codes, to produce a word or phrase, e.g. semantic compaction systems of language representation (Baker, 1994), word prediction (Trnka et al, 2007, 2008), or arrangements allowing individuals to use an Eye-Transfer frame to use gaze to deliver encoded (symbol, word or letter) block selections.
Many dynamic paper-based and powered systems include elements of all three of these organisational systems (hybrids).
“The purpose of a communication display is to arrange language in space so individuals can…] say what they wish to say as quickly as possible, and can do so with a minimal amount of effort.” (Blackstone, 1993)
Symbolic representation
AAC systems offer speech, language and communication access to people at different stages of development, injury or loss. Consequently, different forms of representing language and vocabulary are required.
There are published hierarchies of graphic-symbolic representation. Few have been well researched in terms of their relationship to language, or a person’s cognitive development or decline, or their sensitivity to cultural and linguistic interpretation (see Beukelman and Mirenda, 2013; Sadiku et al, 2022; Tönsing and Dada, 2023).
Use of hierarchies should be adopted with caution (Tönsing and Dada, 2023). Hierarchies pose challenges in terms of deciding how to represent a word or a concept for some individuals. The availability of different graphic-representation systems highlights how vital individualised assessment of language and cognition is for any AAC user, as this will inform SLTs’ understanding of the possible range of sense-making related to symbolic representations (see Murray et al, 2017; Murray and Goldbart, 2009; Stadskleiv et al, 2017;2021; Sutton et al, 2022).
There is emerging reporting of cultural and linguistic consideration for symbolic representation in AAC systems within the UK (see Draffan et al, 2015). The International Society for AAC (ISAAC) has consistently supported international debate on matters of cultural and linguistic appropriateness of symbolisation. ISAAC offers guidance and networks to effectively support people who have a speech, language or communication need in a language other than English.
Literacy development and AAC has received considerable attention in peer reviewed literature. While this guidance does not represent an extensive evidence review, it is clear there is a disconnect between typical literacy achievements, cognitive abilities and AAC skill and knowledge. More could be achieved for AAC users with a developmental or lifelong need for AAC (for more detailed guidance see Clendon et al, 2021; Clendon et al, 2014; Crestani et al, 2010; Smith, 2023).
Communication partners and types of AAC
Unaided AAC systems can be used in any environment, such as in a swimming pool or bathroom. They are spontaneous and facilitate communication between the AAC user and their regular communication partner/s. Unaided systems require a communication partner to understand the person’s communicative meaning and the communication may not be understood by those people who are less familiar with their specific method of communication, e.g. a sign system or sign language.
The use of an aided communication system can support communication to a wider group of people. They can also be used in a wide range of settings, e.g. a paper-based system that is laminated can be used in a swimming pool, or objects of reference can be used to enable someone to be comfortable with what is happening in their world or in their proximity (Buell et al, 2021; Harrison et al, 2021). This can increase independence, particularly for those with severe physical challenges.
Considerations of different forms of AAC supports vary according to communication contexts the person may need, want or aspire to use, including the use of telephone, emails and forms of social media. In this way, output methods support participation in social, educational and work settings.
These methods support the expectation that AAC users can, or can develop the ability to: convey information, e.g. feelings, emotions; chat with friends; ask and respond to questions; give novel information; argue; make a joke; and debate.
AAC is an ever-evolving field and the language we choose to use in describing aspects of AAC or the people who use it can be facilitating or disabling (Robinson, 2022).
A recent debate has offered a further way of considering the key elements of AAC and their relevance to the AAC user, their families, support networks, and professionals. This debate focuses on the four Ps of AAC (Robinson, 2022):
- person – the AAC user
- the communication partner
- and paper and
- powered AAC systems.
According to Robinson, all of the Ps are equal and all have value and use.
AAC need, medical labels and speech and language diagnoses
Speech and language diagnoses and their associated characteristics may be developmental, lifespan or acquired. A key point of debate for more than 20 years has been determining how many people might benefit from AAC and the presenting characteristics of these individuals. An increased understanding of the need for AAC supports service development and provision.
There is a body of evidence that summarises international attempts to quantify the prevalence of people who could benefit from AAC (see Beukelman and Mirenda, 2013; Light and McNaughton, 2012). A UK-based study concluded that while it is difficult to establish need due to the diversity of people who may benefit from AAC, the current best estimate of need for AAC in the UK is about 1 in 200 (Creer et al, 2016; Webb et al, 2023). This is the same as the estimate published by Gross (2010) and is consistent with data from the Health Survey for England (Health and Social Care Information Centre, 2015).
These current figures were established through review of existing literature (epidemiological investigation) and expert opinion. It is important to note that the focus of establishing these figures refers to the need for electronic (powered) AAC, as recommended through specialised provision. Creer et al (2016) acknowledge that whilst these are the most accurate figures on offer, they remain likely to underestimate AAC need, especially in adult social and health service provision. Many individuals who benefit from AAC do not need the input of specialised AAC services, because their needs can be met at a local provision level.
To determine AAC need, prevalence is defined as the number of people who have a particular condition at one point in time. People who could benefit from AAC is defined as people for whom AAC would extend or support their ability to communicate. We acknowledge that describing people who use AAC by their condition is not reflective of how they should be viewed (World Health Organization, 2001) but using such descriptors allows for a level of quantification of need for services.
In the study by Creer et al (2016), specialist providers ranked the most common conditions of people who could benefit from AAC as (ranked in order of need/referral to service):
- Cerebral palsy
- Motor neurone disease
- Stroke/CVA
- Learning disabilities
- Neurodivergent groups including autism and ADHD
- Profound and multiple learning disabilities (PMLD)
- Multiple sclerosis
- Parkinson’s disease
- Alzheimer’s disease/dementia..
The following shows epidemiological rankings: the percentage of the total number of people who could benefit from AAC in terms of the individual conditions (Creer et al, 2016, pp: 650):
- Alzheimer’s/dementia (23%)
- Parkinson’s disease (22%)
- Autism spectrum disorder (19%)
- Learning disabilities (13%)
- Stroke (11%)
- Cerebral palsy (5%)
- PMLD (2%)
- Head/brain injury (2%)
- Other (2%)
- Motor neurone disease (1%)
The epidemiological study shows the main disparities relate to Alzheimer’s/dementia and Parkinson’s disease. They are ranked as the highest expected numbers of people who may benefit from AAC, whilst neither are present in the top five conditions ranked by the specialist AAC providers.
In the summary, 97.8% of the total number of people who could benefit from AAC have nine conditions. The differences in reported clinical-specialist perception of need and prevalence of conditions suggests that:
- there may still be a huge unmet need
- given the rising statistics in the dementias, this may become an increasing need
- the specialist AAC providers’ perceptions of caseload characteristics may vary from local AAC providers’ perceptions of caseload characteristics and AAC needs.
The current estimates provide us with the most comprehensive documentation of AAC need to date, but they are likely to be an underestimation of need.
Having considered the medical terminology associated with AAC need and given that SLTs are specialists in speech, language and communication difficulties, an important consideration is how these conditions may translate into speech and language diagnoses. In understanding this, there will be an enhanced understanding of why individuals presenting with those characteristics may benefit from AAC interventions as part of a holistic speech and language therapy intervention programme.
Regarding a person’s communication needs through a holistic lens, SLTs should consider AAC tools and techniques as potentially supportive to anyone – child, young person or adult – presenting with the following speech, language and/or communication characteristics:
- Aphasia
- Aphonia/dysphonia (including laryngectomy)
- Cognitive communication impairment
- Developmental language disorder
- Dysarthria/anarthria
- Dysfluency (stammer)
- Dyspraxia
- Learning disabilities
- Pre-intentional communication (linked to cognition)
- Speech sound disorders
- Selective mutism
- Social communication disorder.
Unless specifically stated, all definitions apply to developmental, lifespan, acquired presentations and embed consideration of functions of communication, grammar, semantics and pragmatics.
See glossary for definitions and RCSLT clinical guidance for further information.
All forms of AAC systems could be suited to any type of speech and language or medical diagnosis listed. All AAC should be considered on a person-centred, individualised basis as part of a holistic speech and language therapy intervention programme.
Collaboration and co-production
SLTs are specialists in language and communication and a key part of interdisciplinary teams that support AAC assessment, provision, use and support. The practice, research and product field of AAC is an interdisciplinary one. Whilst this guidance focuses on the role and contribution of the SLT, it is crucial to acknowledge that many aspects of AAC service delivery are dependent upon successful interdisciplinary working and co-production with AAC users, potential AAC users, their family members and supporters.
Key professional contributors in a practice context could include teachers, specialist teachers, teaching assistants, occupational therapists, physiotherapists, nurses, healthcare scientists, clinical scientists, psychologists, assistant practitioners, support workers/personal assistants, carers and product suppliers. Professionals can be employed through statutory providers and/or through independent provision. How statutory, independent and private providers collaborate is currently determined at a local level and at times on an individual AAC-user basis.
Collectively, these professional contributors support with:
- understanding the types of AAC available, specifically unaided and aided forms
- understanding of the technology on offer
- the means of accessing AAC
- understanding how AAC supports communication, learning and employment
- understanding how AAC is supported by additional AT tools and techniques
- the means of accessing AAC to support independent or supported living
- the means of integrating AAC with other technologies
- the assessment, recommendation, implementation and review process related to AAC system availability
- understanding of the different funding procedures for AAC across the four nations of the UK.
It is important to recognise that service structures and provision vary across the four countries of the UK. See ‘AAC service structures and provision’ section under Practise guidelines for delivering speech and language therapy service in augmentative and alternative communication for further detail.
The role of speech and language therapy in AAC
The role of the SLT in AAC management is summarised here and detailed in ‘Practice guidelines for delivering a speech and language service in augmentative and alternative communication (AAC)’.
In this context, management considers assessment, provision, implementation and ongoing management.
Assessment
Assessment considers the speech, language and communication abilities and needs of individuals of any age, regardless of whether they have developmental, lifespan, acquired or progressive challenges. From this assessment:
- determine those individuals for whom an AAC intervention will alleviate speech, language or communication challenges
- collaborate with potential AAC users/existing AAC users, family members and other professionals in determining the best AAC recommendation and management plan and to continue to update this plan as necessary
- provide direct therapeutic input for AAC users as long as required to develop their language and communication potential via their AAC system
- carry out regular review of the AAC user’s perspective, functioning and use of their AAC equipment, irrespective of their age, location or access to regular service support. AAC recommendation and provision is typically not a one-off event, but the commencement of life-long intervention support. One AAC user/supporting author commented ‘it gives you a life’
- influence local and national AAC initiatives.
Management
The following points are essential in the AAC management process, but are presented recognising that individual SLTs’ scope of practice or specialist knowledge of AAC will influence level of contribution expected:
- as a minimum, to recognise when an AAC assessment is required and that there are no pre-requisites required for an individual to be considered for AAC
- to recognise the referral processes and/or criteria for specialist services in their country or region of the UK
- to understand what a comprehensive assessment for AAC should include
- to lead or facilitate appropriately detailed AAC assessments
- to lead or contribute to the process of AAC recommendation/s, considering all relevant options and not just already-known options
- to liaise with specialised AAC and AT service providers (or if a specialised SLT to liaise with local services as per referrals)
- to lead and work collaboratively on AAC implementation processes for as long as is needed for the AAC user to achieve their potential with AAC tools and resources (including supporting language development or maintenance of language skills via AAC). This may include identifying an AAC champion to support ongoing needs
- to support access to funding for AAC when potential users do not qualify for NHS provision
- to lead or contribute to ongoing AAC training and support for AAC users, family members and staff
- to ensure maintenance and repair of AAC devices via services responsible for the management of medical devices
- to lead reporting of AAC clinical outcomes, including reporting of unmet needs
- to facilitate AAC user review processes by recognising changing AAC needs across the lifespan
- to recognise user and family support needs across the lifespan by signposting access to AAC role models, signposting to (re)accessing AAC services, community teams and other outreach initiatives
- to be responsible for maintaining and developing personal AAC clinical skills and knowledge
- to influence more broadly by engaging with local and national initiatives that include reviews of:
- UK service structures and provisions, e.g. local, specialist, specialised provision and independent/private provision
- AAC standards of practice, including NHS and non-NHS locations of practice
- legislation and policy that impacts AAC users, families and service structures
- AAC research and development priorities and associated funding opportunities.
Practice guidelines for delivering a speech and language service in augmentative and alternative communication (AAC)
The RCSLT makes the following recommendations for delivering a speech and language therapy service in AAC.
As stated in ‘AAC in context – supporting diversity’ searching a scattered evidence base (Schlosser et al, 2005) is one of the recurring themes when reviewing types and levels of evidence for AAC management.
There are a limited number of studies investigating the personal impact of AAC, assessment and intervention approaches (see resources page ).
It would be easy to dismiss the limited literature, but it is pleasing to see the extent of this ever-growing evidence base. There are challenges in appraising assessment parameters or intervention options due to the breadth of AAC influence. SLTs may work with a range of individuals, including:
- a young child with a range of characteristics that impact on their speech, language and communication development
- an adult with challenges that have impacted upon them across their lifespan
- an adult with an acquired communication challenge
- an individual with a progressive or life-limiting condition.
All of these individuals operate in a wide range of contexts that include community, early years, educational, social services, work environments and hospital settings. To appraise the AAC evidence base as it applies across all of these contexts and potential characteristics of the AAC users is a big task.
We have been systematic in our process of reviewing available evidence by using key search terms and appraisal tools to complete a literature review. We have not completed any systematic literature reviews as they would fail to generate sufficient breadth of information about current influencers of practice and ongoing research priorities in the field of AAC. Therefore, in adopting a systematic approach to appraising the literature by identifying a search protocol, the following sections highlight the type and level of evidence available. (See ‘how we develop our guidance’ for more information.)
The guidance has been organised into key sections of consideration for any speech and language therapy services’ remit in AAC. We recognise that the term ‘service’ has different connotations. A service may involve one clinician in statutory or independent/private practice through to an extensive team of SLTs with a broad geographical reach and/or a multidisciplinary team that includes an SLT, for example, in an ‘early supported discharge’ stroke team.
How to use the guideline statements
The 16 guidelines are worded so that SLTs can consider them during the range of interventions they may provide for potential or existing AAC users, families and supporters. They are not listed in any hierarchical fashion. Each guideline is associated with a particular theme of AAC practice. There are seven themes of practice:
- AAC user identity
- Awareness of AAC, skills, knowledge and clinical competencies
- AAC service structures and provision
- AAC assessment, recommendation and provision
- AAC intervention/management
- Conversation partner training and support
- Managing transitions
Download a summary document of the seven themes of AAC practice and related guideline statements
AAC user identity
- Guideline 1: Speech and language therapy services should be mindful of the identities, roles and contributions of the AAC users of the service by supporting access to interventions that are timely and individualised.
- Guideline 2: An AAC system is often for life, regardless of the age at which it is introduced and may take time to learn. This should be factored into the ongoing management and support of the AAC
- Guideline 3: Awareness of everyone’s linguistic and cultural influences should be recognised in any decision-making process. Consider AAC language representation options, language output options and, if using electronic options, available accents and opportunities for voice banking/donor voices
The premise of much AAC intervention is lack of attainment, inability or loss and is often seen as an option that is the last resort, prizing any other forms of communication above it (e.g. Goldbart and Marshall, 2004; Iacono, 2019; Romski and Sevcik, 2005). There remains a perception that use of AAC will prevent speech development or recovery (Romski and Sevcik, 2005) or language and communication skill development or recovery (Smith, 2015). There is sufficient evidence and assurances to dispel these perceptions of AAC as the last resort as being ill-conceived myths (see Romski and Sevcik, 2005).
Another key factor is the approach to collaborative practice and where the AAC user and family members contribute to that process. A frame of reference that is not about deficit but about equal, diverse and inclusive possibilities alters perspectives on AAC and what it means to be an AAC user. Re-framed AAC can instantly be a window into what can be achieved rather than what might be absent. As an example, ‘difficulties in social interaction’ could be re-created as ‘opportunities for social connectedness’. The lack of or loss of identity (as a non-speaker) can be turned around, for instance ‘I am proud to be a communication aid user, it makes me who I am’ (Moulam, supporting author and AAC user).
The road to becoming an AAC user is not without challenge, with the terms ‘acceptance of changed identities, time, persistence and resilience’ appearing in many accounts (Smith and Murray, 2011). Accounts from family members attest to their fortitude and determination to often access AAC services and maintain that support over time (Goldbart and Marshall, 2004). As evidenced by a parent supporting author of these guidelines, fortitude may be required to access NHS continuing healthcare (CHC, England) where an AAC user can be scored as having no ongoing need in the “communication” domain because they use AAC and are mis-perceived as having no ongoing AAC/communication support needs.
Where the AAC user has an effective picture-graphic system that enables communication, that AAC system should follow them and not be changed because they move environment or location and/or the support team has a preference for a different system.
As AAC primarily acts as a medium for conveying the speech, language and communication intentions of the user, nuanced to their linguistic and cultural context, it is important to consider these elements of identity when considering the type of AAC system and its attributes (Pert, 2022; Tonsing and Soto, 2020).
See Finding a voice for Richie as an example.
Awareness of AAC skills, knowledge and clinical competencies
- Guideline 4: Appraise yourself of the Communication Access UK (CAUK) training and encourage service providers to consider it as mandatory training content for all staff.
- Guideline 5: Individuals, service managers, service providers, commissioners, and education and training providers should draw on the resource Informing and Profiling AAC Knowledge and Skills (IPAACKS and derivations of) as an evidence-informed template to appraise and develop AAC skills, knowledge and provision.
Communication disability is an under-recognised entity, with AAC users in particular being treated differently in general community contexts – see Ableism and communication impairment (Beth Moulam).
Communication Matters UK introduced the concept of the Communication Access UK project. This led to a UK-wide partnership, including the RCSLT, aiming to improve the lives of people with communication difficulties by promoting communication accessible organisations and social contexts. This project offers freely available, on-line training to enhance everyone’s understanding of communication difference and how to support those individuals. Completion of the training leads to individual or organisational accreditation.
Skills, knowledge and clinical competencies in AAC can be appraised in several ways. IPAACKS is a resource that can be used in several ways and for a range of purposes, by individual workers, service providers, organisations and AAC users (see table 3). The key aim central to IPAACKS delivery is to improve the experiences, opportunities and quality of life of AAC users.
Table 3: Ways to use IPAACKS
| Who? | What? | Why? |
|---|---|---|
| Individual workers | To consider the elements involved in delivering quality AAC services | To help understanding of values, knowledge and skills base required to provide a quality service to AAC users |
| Individual workers and their managers or supervisors | To explore the components involved in being a skilled and knowledgeable AAC worker | To identify an individual worker’s strengths and gaps in knowledge and skill |
| Organisations | To explore what aspects of a comprehensive AAC service is in place, emerging or absent | To identify staff development needs of teams supporting AAC users, as well as inform service planning |
| Education and training providers | To explore aspects of an accredited curriculum that includes AAC or bespoke training content | To inform the content of vocational, undergraduate and postgraduate education and training in AAC |
| AAC users, their families, personal assistants and carers | To explore the extent of an AAC service | To ensure they understand the full extent of support that they can expect throughout their lives and to enable them to check that the team around them includes the range of expertise that they need |
In brief, the IPAACKS manual covers two broad areas
- Core values
- AAC specific skills and knowledge
The core values and commitments outlined are required of any worker, but essential when supporting AAC users. For example, respecting diversity, challenging inequality and promoting opportunity, and promoting inclusion and participation. They mirror many professional or sector-based frameworks on quality service provision. The AAC skills and knowledge strands describe the characteristics of workers who are involved in AAC. The AAC specific strands are more role specific; where some workers will need to evidence knowledge and skills in all of the AAC strands, others will only require some AAC specific strands. There are eight AAC specific strands:
- identification of need
- AAC assessment
- implementation
- review
- technology (preparation, adaptation and integration)
- technology (management of resources)
- AAC leadership
- facilitating AAC learning
There are four levels of knowledge and skill across the eight strands. These levels support appraisal of SLTs at very different stages of their career, e.g. from newly-qualified to highly-specialist SLTs. This framework also acknowledges the multidisciplinary components of AAC working. Some SLTs will score in every section, others will not have or never have that particular AAC remit. This UK-devised resource specifically focused on AAC competencies across stakeholder groups. Training on the use of IPAACKs may be provided as an aspect of specialised AAC service support. Derivations of competency frameworks may be available locally. The IPAACKs levels may also resonate with other terminology used across services, e.g. supportive, assistive, registered, enhanced, advanced and consultant practitioners.
AAC service structures and provision
- Guideline 6: Awareness of AAC service structures and provision locally, nationally and UK-wide will inform referral procedures and intervention options that are inclusive of the service user perspective.
- Guideline 7: Awareness of transdisciplinary contributions to the AAC management process will ensure AAC users, families and supporters access a holistic appraisal of their AAC needs.
Many aspects of AAC service delivery are dependent upon successful interdisciplinary working and co-production with AAC users, or potential AAC users, their family members and supporters, as well as service providers.
Key professional contributors in a practice context include teachers, specialist teachers, teaching assistants, occupational therapists, physiotherapists, nurses, healthcare scientists, clinical scientists, healthcare scientists, psychologists, assistant practitioners, support workers/personal assistants, carers and product suppliers.
Professionals can be employed through statutory providers and/or through independent practice. How statutory, independent and private providers collaborate is currently determined at a local level and at times on an individual AAC-user basis.
Collectively, these contributors support understanding the types of AAC available, specifically unaided and aided forms:
- understanding of the technology on offer
- the means of accessing AAC
- understanding how AAC supports communication, learning and employment
- understanding how AAC is supported by additional AT tools and techniques
- the means of accessing AAC to support independent or supported living
- the means of integrating AAC with other technologies
- the assessment, recommendation, implementation and review process related to AAC system availability
- understanding of the different funding procedures for AAC across the four nations of the UK.
Service structures across the UK
It is important to recognise that service structures and provision vary across the four countries of the UK. For example, in Scotland there is one national NHS service that covers adults and children for 12 out of the 14 health boards. Another national service (education) covers commissioned areas to support children in access to education with a cross over to AAC. The remaining two health boards have local specialist services. They work collaboratively with the local providers. There are no specific referral criteria.
By contrast, England offers a hub and spoke structure, where the AAC specialised services (14 in total: three north, three middle, four south and four in London) act as the hubs covering 10% of the AAC population who meet strict referral criteria. The remaining 90% of AAC users in England are supported at a spoke (or also include a local) level through various funding routes, including the NHS and education, independent/private or charitable organisations.
In Wales, there is one National Electronic Assistive Technology (EAT) service offering assessment and provision for electronic AAC. Local specialist SLT AAC services, employed by each health board, provide a range of non-powered AAC solutions. There are criteria for referral to both local and national services. All funding routes are via NHS Wales.
In Northern Ireland there are five health and social care trusts and one regional specialist AAC service. There are specific referral criteria for the specialist regional service; however, SLTs within the trusts and the regional team work collaboratively to manage and support AAC users.
Where funding is required, there may be local, regional and national procedures that all SLTs – whether NHS, education or social services employees or independent – should acquaint themselves with. Most national or regional hubs offer training and CPD updates for SLTs and in some cases for any party with an interest in AAC.
As national and local provision varies, for relevant policy and legislation in each country see the resources page and RCSLT policy and influencing web pages. For more information on specialist AAC provision, interdisciplinary contributions to supporting AAC identification and use, see Communication Matters resources:
Collaborative working
There are various models of working (e.g. Glennen and DeCoste, 1998). Local SLTs may work autonomously within a multidisciplinary team, where their role and contribution is clearly defined, and may involve reporting from a profession-specific perspective. This type of working may result in a referral to specialised AAC teams, but this will not always be necessary. However, there may be opportunities for working in more integrated and collaborative ways. These may be described as:
- An interdisciplinary approach: involves team members from different professional disciplines working collaboratively, with a common purpose, to set goals, make decisions and share resources and responsibilities. This may be observed when local and specialised AAC provision collaborate.
- Transdisciplinary work: surpasses interdisciplinary work in that it seeks to develop holistic perspectives by integrating different disciplinary perspectives, thereby creating new frameworks to understand problems for the purposes of developing solutions. Specialised AAC provision typically aspires to work in this way, but this approach can also be observed in some local specialist AAC provision.
- The integration of services and collaborative practices, e.g. statutory, charitable and independent providers, is a developing landscape as more providers offer alternatives to the more traditional NHS SLT role/input.
AAC assessment, recommendation and provision
- Guideline 8: AAC assessment referrals and final recommendations should be based on consistent reporting of speech, language and communication characteristics. Reporting should include consideration of all forms of AAC, vocabulary selection and, in aided forms of AAC, vocabulary organisation, graphic representation options and trajectory plans.
- Guideline 9: Familiarise yourself with key AAC assessment frameworks and support tools and apply them to your appraisal of individuals who may benefit from AAC.
- Guideline 10: AAC recommendations need to be recorded for future appraisal of outcomes. AAC recommendations should be shared amongst all members of the team supporting the individual.
Generic assessment: Whilst elements of an AAC assessment include speech, language and communication appraisal, it differs in its methods from assessing an individual who can name, point to or describe something using typical unaided methods of speaking and communicating. This does not mean it is impossible to comprehensively appraise the speech, language or communication skills of someone who might benefit greatly from an AAC system. An effective appraisal of these skills or challenges are key to an effective AAC assessment and are the core contributions to be made by any SLT as specialists in this aspect of an AAC assessment. Currently, there are no or limited speech, language or communication measures that have been standardised on children or young people who typically benefit from AAC Those with developmental language disorder (DLD) may consider Clinical Evaluation of Language Fundamentals (CELF) (Semel et al, 2004). Standardised measures of ability in individuals post stroke or with acquired dysarthria do exist and are useful in the SLTs’ AAC assessment toolbox. For example, the Comprehensive Aphasia Test (Swinburn et al, 2004).In the absence of such resources for all age groups, in an AAC context we can use standardised measures, but use them descriptively. From the literature, we find that use of such measures, where physically possible, or possible with minor adaptations, e.g. by placing standardised picture material on an Eye-Transfer (E-Tran) frame, is acceptable and justified. This practical approach to assessment enables the consistent description of abilities or challenges at a given point in time, as well as describing changes over time (Broberg et al, 2012; Broomfield et al, 2019; Smith, 2023). Current evidence suggests a lack of consistent description of presenting language and communication abilities in AAC users (Murray et al, 2019; Lynch et al, 2019).Whilst there may be an absence of standardised measurement, there is an abundance of:
- developmental checklists
- language comprehension checklists
- communication checklists
- pragmatic profiles (AAC)
- communication function checklists
- speech and communication scales
- quality of life checklists
- language of daily living checklists.
They are mostly developmentally oriented and based on our understanding of typical development. All can support detailed descriptions of an individual’s current speech, language and communication abilities, differences and challenges. These can provide summaries of an individual at a point in time. There is an important caveat: not all individuals who may benefit from AAC will identify as having communication challenges, but rather having different ways they prefer to communicate. Existing checklists may be unhelpful as a way of describing such communication preferences. These assessment resources and the reports produced from them will inform the AAC recommendations. Although not an exhaustive list, these recommendations will provide insights into:
- the perspectives, preferences and expectations of the person who will use AAC, their family members and supporters
- the multimodal aspects of communication and the range of AAC systems that may be helpful to an individual user, e.g. an AAC package may eventually include objects of reference, key word sign and a tablet device
- the embodiment of unaided forms of communication as core to the user’s identity, e.g. gesture, vocalisation, facial expression
- the range of vocabulary that an AAC system should offer the user
- the way that vocabulary should be (visually) represented for the individual (e.g. written, graphic, photographic or real object)
- how the vocabulary can be organised (columns may best suit some, rather than rows)
- the preferred or possible method/s of accessing any aided AAC
- the use of text-to-speech options
- how the chosen vocabulary should be able to support the individual as they develop or as they regain or lose language abilities.
AAC recommendations can be achieved by using:
- perspectives of potential AAC users, family and supporters
- existing speech, language and communication standardised measures (with the modifications suggested)
- checklist summaries (as suggested)
These elements should be incorporated into anyone’s AAC speech, language and communication recommendation report. Consideration of all forms of AAC, with no pre-requisite skills required, will inform the final recommendation. Such recommendations may be produced at local, regional or national levels depending on service organisational parameters.
AAC-specific elements of assessment
The following are the AAC assessment tools with some evidence base or clinical traction in the UK:
Communication Competence: A key AAC assessment framework that is strongly embedded in the clinical process of assessment and recommendation is the Janice Light model of Communication Competence (Light et al, 1987-2019). It has four key elements of competence defining the operational, linguistic, strategic and social competencies of an AAC user. Latterly it has also considered the context of use. This has an extensive publication base and offers differing levels of evidence in its outputs, but must be recognised for a bias towards electronic AAC systems, leaving less commentary related to the benefits of paper-based systems. It is also focused on the AAC user’s competencies and does not entirely consider the wider context or the competencies of the communication partners. One key element it emphasises is linguistic competence. Appraisal of this element is a key contribution to be made by any SLT and should be supported by the use of techniques suggested in the preceding section about speech, language or communication assessment.
Identifying Appropriate Symbol Communication (I-ASC): A more recent framework that is supporting assessment and clinical decision making is the I-ASC Explanatory Model of clinical decision making (Murray et al, 2019; Lynch et al, 2019). It is based on extensive UK research, with a good publication base and offers a framework for exploring the holistic elements involved in an AAC assessment and recommendation process. Its findings are biased towards children and young people and electronic AAC. It offers a structure for assessment that looks beyond the AAC user to all potential influencers on a final recommendation and intervention plan, e.g. staffing support, attitudes and skills, and periods of transition. Its structure may be of relevance beyond children and young people.
Means, Reasons and Opportunities: This is another model for exploring what an AAC system might offer someone to consider for their communication. Whilst this appears to have considerable clinical traction, there is a non-existent research evidence base for its influence within AAC recommendations.
- See A Grain of SaLT
The Participation Model: A framework for exploring the components of an AAC assessment (Beukelman and Mirenda, 2014). The participation model focuses on assessment as a dynamic process that needs revisiting as people learn new skills or as their situation progresses, in other words, whenever there are changes in participation levels. Assessment is broken up into four stages:
- Identifying whether or not the person has complex communication challenges
- Assessment that considers both access and opportunity barriers that are impacting on their participation
- Planning the scope and sequence of intervention
- Monitoring progress in terms of how students are participating in their environments
- See The Participation Model
The Communication Matrix: This is a framework for identifying how a person is communicating and from that developing a plan for logical communication goals (Rowland et al, 2016; Quinn et al, 2021). Originally designed to explore the expressive communication skills of children with profound and multiple disabilities. As stated in the handbook, the Matrix is appropriate for individuals of all ages who are at the earliest stages of communication: “…the range of communication skills that the Matrix covers would occur between 0 and 24 months of age. The Matrix accommodates any type of communicative behaviour, including “augmentative and alternative” forms of communication (AAC) and pre-symbolic communication (such as gestures, facial expressions, eye gaze and body movements)…The Communication Matrix is NOT suitable for individuals who already use some form of language meaningfully and fluently.” (Rowland, 2014, pg 4).
There are two resources in common use in the UK that support decision making and AAC recommendations:
Talking Mats: An AAC user decision-making tool (Murphy et al, 2013). Talking Mats is not an assessment framework or a communication system, but is a key decision-making tool to support AAC users and family members to identify what is important for them. With a good publication base, it may act as a useful tool during an assessment, recommendation or intervention process.
Communication Passports : Personal communication passports are a practical and person-centred way of supporting children, young adults and people who cannot easily speak for themselves (Millar and Aitken, 2003). It is particularly helpful, but not exclusive to, appraising the needs, communication abilities and preferences of those with profound and multiple learning disabilities, severe learning disabilities and, in some instances, those who identify as neurodivergent.
Passports:
- present the person positively as an individual, not as a set of ‘problems’ or disabilities
- provide a place for the person’s own views and preferences to be recorded and drawn to the attention of others
- reflect a ‘flavour’ of the person’s unique character
- describe the person’s most effective means of communication and how others can best communicate with and support the person
- draw together information from past and present, and from different contexts, to help staff and conversation partners understand the person, and have successful interactions.
AAC recommendations made by SLTs: Recommendations for AAC systems need to be evidence based. Evidence suggests that AAC recommendations are complex and require a balancing of potential trade-offs. For example: best language representations system over local knowledge of language representations systems; cost over regular replacement; or, the best system for now over how it may suit as things progress or deteriorate. These trade-offs are real and impactful. For these reasons, we need to be mindful of how we record AAC-related assessment and recommendations, so they can inform later intervention evaluations. Outcome measurement tools exist to support accurate appraisal and reporting and include:
- Therapy Outcome Measurement – AAC (TOMs-AAC, Enderby, 2014). This has been identified specifically as the key tool to use for AAC related activity in the UK
- The Family Impact of Assistive Technology Scale for Augmentative and Alternative Communication (FIATS-AAC), g. Fjeldvang et al (2023).
At present there is ongoing work exploring the development of a patient-reported outcome measure in AAC (PROM-AAC, Broomfield et al, 2019).See RCSLT information on outcome measurement.
AAC intervention/management
- Guideline 11: SLTs should be appraised of the range of intervention strategies that are available to support the language and communication abilities of AAC users.
- Guideline 12: Within AAC user intervention contexts, SLTs should apply language and communication interventions that are used in contexts where AAC is not regularly needed, e.g. developmental language disorder.
Some implementation considerations for AAC use
AAC tools and techniques can promote relationships, social inclusion and facilitate participation so that individuals can develop or maintain communication in different settings. The AAC system can be used as an embodied alternative to speech or as a scaffold to communication between the AAC user and their conversational partner/s, where either party accesses elements of the AAC system in a co-constructed manner facilitating an agreed meaning (Smith and Murray, 2016).
While this is often a daily interaction approach for AAC users, this approach is often observed during therapeutic interventions with any communication disability. For example, people living with stroke, motor neurone disease or other acquired communication challenges benefit from this co-constructed scaffold for communication success (May et al, 2023; Smith, 2023).
Following a review of the literature, the following implementation approaches and strategies were coded according to level of evidence. The approaches considered apply to aided communication only.
The information presented may apply to all people and so it is not organised according to developmental, lifespan, acquired or progressive communication needs. Information is organised thematically and is not indicative of any prioritisation of approaches to consider. The elements of intervention include focus on the aim of the intervention approach and in some instances include particular tools that would be used to support the intervention approach, e.g. approach – aim to understand cause and effect; tools – switches.
Table 4 provides a summary, further detail of each approach is provided in the reference list and resources webpages.
Table 4: Implementation approaches and strategies to support AAC skill development, and their evidence base (N.B. references themed according to the sections below are provided in the references.)
| Organisation of vocabulary (non-powered and powered) | |||
| Type | Description | Level of evidence (due to types of studies) | Reference sources |
| Encoded | Semantic compaction | Moderate | Empirical, practice and user accounts |
| Semantic/schematic | Core and fringe | Limited | Practice and user accounts |
| Visual scene display | Good | Empirical, practice and user accounts | |
| Phrase-based display (not to be confused with Gestalt language processing) | Limited | Empirical, practice and user accounts | |
| Taxonomic and/or semantic | Pragmatic organisation (PODD) | Moderate | Empirical, practice and user accounts |
| Taxonomic and/or semantic | Grid displays | Moderate | Empirical, practice and user accounts |
| AAC-specific teaching and learning methods (non-powered and powered) | |||
| Type | Description | Level of evidence (due to types of studies) | Reference sources |
| Language interventions | Aided Language Stimulation (may also be referred to as modelling) | Good | Empirical, practice and user accounts |
| Conversational scaffolds and ramps | Moderate | Empirical, practice and user accounts | |
| Narrative therapy | Good | Empirical, practice and user accounts | |
| Semantic, conceptual and grammatical approaches (may also be referred to as modelling) | Moderate | Empirical, practice and user accounts | |
| Motor patterning | Language Acquisitions through Motor Planning (LAMP) | Moderate | Empirical, practice and user accounts |
| Cause and effect | Use of switches | Moderate | Empirical, practice and user accounts |
| Partner-assisted (intervention) communication approaches | Intensive interaction | Moderate | Empirical, practice and user accounts |
| Objects of reference | Moderate | Empirical, practice and user accounts | |
| Picture Exchange Communication System | Accounts suggest: Open to question/Evidence debated | Empirical, practice and user accounts | |
| Person-centred design/participatory interventions | Communication passports | Limited | Practice and user accounts |
| Communication dictionaries | Limited | Practice and user accounts | |
| Lesson plans from specific supplier websites | Teaching and learning strategies for specific dedicated AAC systems | Limited | Practice and user accounts |
| Non-AAC-specific teaching and learning methods, that resonate with AAC intervention objectives | |||
| Type | Description | Level of evidence (due to types of studies) | Reference sources |
| Person-centred design/participatory interventions | Language intervention and cultural awareness methods
|
Moderate | Empirical, practice and user accounts |
| Parent-child interaction | Moderate | Empirical, practice and user accounts | |
| Grammar | Interventions in DLD and dosage considerations | Good to moderate | Empirical, practice and user accounts |
| Colourful semantics | Moderate | Empirical, practice and user accounts | |
| Text-to-speech and social media platforms | Screen readers, prediction software, video and text-based interaction platforms | Moderate | Empirical, practice and user accounts |
This demonstrates that there is more than one approach to support language and communication development in aided AAC users. It is important to remain appraised of differing approaches as this will influence your clinical decision making and management plans. For a detailed review of considerations of:
- unaided AAC – see Grove and Launonen (2019); Lacey et al (2017); Moorcroft, et al (2019)
- semantic, conceptual and grammatical AAC interventions – see Smith (2015); Sutton et al (2022)
- symbolic representation – see Murray et al (2016); Porter and Burkhart (2010); Tönsing and Dada (2023)
- participatory-access methods for any AAC system – see Buchholz et al (2019); Hemsley et al (2015); Hynan et al (2014); Waller (2019)
Conversation partner training and support
- Guideline 13: There is a variety of evidence-based communication partner training programmes and strategies that have been developed to support communication between AAC users, families, supporters and professionals. It is important SLTs understand what is available to support the AAC users and their communication partners.
- Guideline 14: Communication partner training programmes have been shown to enhance the interaction and engagement of AAC users and reduce their anxiety and stress when communicating. Ensure that partner training forms part of any AAC intervention plan.
Given the reach of AAC, we must recognise the breadth of potential conversation (communication) partners for someone who may benefit from AAC. In this guidance, we attempt to cover considerations from infants through to older individuals who may have different challenges impacting on their relationships, their communication and how this is accommodated (Giles et al, 1991).
In the context of the communication partner/s, we must consider their knowledge, understanding and attitude (Ball and Lasker, 2013; Dooley et al, 2015; Kent-Walsh et al, 2015; Lynch et al, 2019; Ogletree et al, 2016, 2022; Shire et al, 2015); and at the same time understand what AAC users might want from a communication partner (Grove and Launonen, 2019; Midtlin et al, 2015).
Those contexts for communication and conversation are so diverse that it is a challenge to capture them in this summary.
Types of communication partner
Communication partners vary but include the general public, family members, carers, friends and peers, educational, healthcare and social services professionals, as well as employers and employees. The type of communication partners and the settings in which communication occurs are important to consider in communication partner training. Communication partners are frequently unprepared for how to support effective AAC-mediated communication, partly due to limited training on how to use compensatory strategies to support interactions (e.g. Kent-Walsh et al, 2015; Murray et al, 2022).
Types of training approaches
Training approaches to enliven communication partners’ understanding of what to do and how to do it may focus on:
- seeking an understanding of the many ways in which AAC users may engage and communicate
- seeking an understanding of what different communication signals and methods may be indicated by the AAC user
- giving AAC users sufficient time to communicate and/or converse
- seeking the AAC users’ views on how best to communicate with them
- conversational scaffolding techniques, including re-casting or re-voicing (speaking on behalf of) messages mediated by AAC
- believing the messages offered and co-constructing an agreed understanding of them
- modelling good communication strategies for conversation partners to be aware of and use
- offering ongoing support for the AAC user and their communication and conversation partners as things change, which may be due to improvement in or loss of speech or language or communication skills
- recognising that clear message transmission is not always easy and how to navigate those convoluted transmissions
- following the AAC users’ reminiscences of what is important and meaningful to them.
There are several conversational partner training programmes, initiatives and suggestions (e.g. Douglas et al, 2022; Hayes and Traughber, 2021; Murray et al, 2022; Ogletree et al, 2016; Starble et al, 2005; Thiessen et al, 2013, Volkmer, 2020).
It is clear from a review of the literature that it is important to be mindful of the specific AAC user’s context and how communication partners need to be adaptable and flexible to enhance communication and conversational success. The AAC user is already working hard enough.
Managing transitions
- Guideline 15: In every AAC decision-making encounter, anticipate transitions and changing needs. Take considerable advice on potential changes to the AAC user’s characteristics and needs, as well as any technology change and development. In doing so this will lead to the best-informed speech and language therapy recommendations, and choices for the AAC user.
- Guideline 16: Keep detailed records of AAC decisions, so that at transition points the AAC user can continue to move forward, rather than repeat what may have happened in the past.
Anticipating transitions in the life of an AAC user is paramount. Transitions will happen for all AAC users, whether that be:
- leaving hospital
- changing classroom, school, or college
- changing educational, health or social services support teams
- changes to family and home circumstances
- changes to work patterns
- changes to the AAC system
- changes to AAC needs
“Finding a communication system that is… right for today, tomorrow and the day after tomorrow.” (Beukelman and Mirenda, 2013)4
This statement sums up the long-term commitment required of AAC services and the SLT role within that. Needs change. This may happen on a micro-level, such as changing class, or on a macro-level, such as changing an AAC system due to system obsolescence. It is important to consider and predict/anticipate, the consequences of change and transition. In doing this we will be better prepared to ensure that there is not a hiatus, or loss, for the AAC user. It is key to:
- ensure new people around the AAC user understand their communication methods and needs
- choose to use reliable and proven technologies
- not be beguiled by mainstream technologies when a dedicated AAC system and/or device solution may better support the AAC user now and in the future
- share information about individual circumstances
- manage routes of discharge from a service to efficient re-referral
Future planning includes expected change, how you intend the future AAC system to look and function, and how the person may be communicating. It also includes changes in the environment or setting such as changes in educational provision or staff providing services. Evidence suggests that predicted change in the person’s future influences decision making (e.g. Dada et al, 2021; Lynch et al, 2019; Webb et al, 2021, 2023). A recommendation from this evidence is to ensure that information about communication needs and plans flows from existing to new settings.
See information on transitions from I-ASC (Identifying Appropriate Symbol Communication).
Regarding technology change, this is an inevitable aspect of aided AAC work and is often welcomed. However, for those long-term users of AAC it can pose some significant challenges. Be mindful of how to navigate differing expectations based on overall awareness and experience of technology. Engage in discussion to ensure a shared understanding and expectation of AAC. This should include how dedicated AAC technologies relate to off-the-shelf technologies.
Where decisions are delayed due to expected updated versions of the technology, ensure existing systems remain adequate to support needs in terms of communication and language development.
Glossary: key terminology and their descriptions
This glossary is not exhaustive, but includes key terminology and their descriptions. Terminology across the field of AAC is vast, not always clear and can be confusing and ever changing. We have attempted to share definitions of synonyms (old, current and aspirational).
In the resources page, we include links to various websites who provide their own AAC related terms, e.g. Communication Matters; Ace Centre.
Augmentative and alternative communication (AAC) is a set of tools and strategies that an individual uses to solve every day communicative challenges. Communication can take many forms, such as speech, a shared glance, text, gestures, facial expressions, touch, sign language, symbols, pictures, speech-generating devices, etc. Everyone uses multiple forms of communication, based upon the context and our communication partner. Effective communication occurs when the intent and meaning of one individual is understood by another person. The form is less important than the successful understanding of the message.
See International Society for Augmentative and Alternative Communication: About AAC
The terms augmentative and alternative typically describe a continuum of communication options. There is ongoing international debate about the meaning of these terms. Here are the most typically used definitions:
- Augmentative – may support existing forms of communication
- Alternative – may be used instead of speech
Access method refers to the method by which an individual accesses their communication system. Also known as the selection method.
Aided communication involves the use of physical tools and techniques. These can include paper-based materials as well as electronic devices. Aided communication methods are rarely as quick as an unaided method, but may offer more communication independence.
Alternative access involves ways for a user to use AAC when they cannot point. These may include eye-pointing, partner-assisted scanning (using the communication partner’s finger) Eye-Transfer (E-Trans) frames, switches, joy sticks, head mouse, etc. This is also called indirect access.
Communication device may refer to any paper based or electronic AAC system. The ‘device’ could describe a communication book or folder or an electronic AAC system. It is more typically used to describe an electronic AAC system.
Communication partner is anyone that a person using AAC communicates with. This interaction may relate to personal needs and requests.
Communication system describes the elements of type of graphic-symbol representation, the mode of organising and storing these representations and any related attributes of the system, e.g. is it a folder, a board, an electronic device, how does the user access it?
Conversation partner is anyone that a person using AAC has a personal or relationship-based interaction. Partners can be both communication partners and conversation partners.
Conversation training/Conversation partner training describes a range of documented approaches targeting communication partners of AAC users. All aim to support partners to understand why differing communication or conversational strategies may be required and how to deliver supportive communication approaches to support the AAC user to demonstrate their abilities, wants and needs.
Direct access is when the AAC user points to the page or screen with their finger (or some other part of their body, e.g. knuckle, elbow, toe).
Encoded language is when codes stand for words or phrases, e.g. LOL for ‘laugh out loud.’
Electronic AAC means the same as ‘powered AAC’ (see below for details).
Expressive language is the language we use to communicate with or talk to others. Anything we use to get a message across to other people. It is the opposite of receptive language (see below).
Eye gaze “or eye tracking is a way of accessing your computer or communication aid using a mouse that you control with your eyes… eye gaze systems work by having lights and cameras that are constantly sending and receiving information. The camera picks up light reflections from your pupils and translates the movement of your eyes into mouse cursor movements.” (Inclusive What is Eye Gaze?)
Eye pointing “serves the same function as finger pointing. For example, by looking between an object and their partner, a child might signal that they are interested in or want to play with that object. Eye-pointing is described as “The context-relevant, controlled and intentional use of gaze in order to direct one or more partner’s visual attention to any item or object for a deliberate communicative purpose. Other communication modes (facial expression, vocalization, head movement and body position) may be employed, as available, to support the use of gaze” (Sargent et al, 2013).” (UCL What is eye-pointing?)
High-tech AAC is AAC that uses a battery. This is an old term, most people in the UK now use the term ‘powered AAC’ or ‘electronic AAC’ instead of this.
Indirect access is a way for a user to use AAC when they cannot point. These may include eye-pointing, partner-assisted scanning (using the communication partner’s finger,) Eye-Transfer (E-Tran) frames, switches, joy sticks, head mouse, etc. This is also called alternative access.
Language representation system refers to the way in which concepts, ideas and words are represented for the AAC user. This could include key word signs, a sign language, written words, photos, real objects and graphic symbols.
Low-tech AAC is any AAC that does not have a battery. This is an old term, most people in the UK now use the term ‘paper-based’ or ‘paper AAC’ instead of this.
Message banking necessitates you using your own voice to record stories, phrases, words and/or sounds which are saved, stored and then played back to support your communication in time to come. When they are played back, the stories, phrases, words and/or sounds will sound exactly as they did when they were recorded.
Mounting system (for an AAC system) refers to specialised equipment enabling the AAC system (paper based or electronic) to be fixed to the AAC user’s wheelchair, bed, table, etc. to support access to the AAC system.
Neurodivergent, sometimes abbreviated as ND, means having a mind that functions in ways which diverge significantly from the dominant societal standards of “normal” (Walker, 2021, pg 25-33).
Neurodiversity is the diversity of human minds, the infinite variation in neurocognitive functioning within our species (Walker, 2021, pg 25-33). It applies to us all.
Neurotypical, often abbreviated as NT, means having a style of neurocognitive functioning that falls within the dominant societal standards of “normal” (Walker, 2021, pg 25-33).
Non-powered solutions (may also be referred to as paper solutions or light-tech or low-tech solutions) includes communication charts or boards, and notebooks or folders with no electrical or battery power supporting their use. Vocabulary provided in these paper-based systems can be as extensive and as complex as many electronic systems. Included in these non-powered solutions are the use of real objects as communication referents, and word or picture materials that act as conversational scaffolds. Also included here would be platforms for presenting aided materials, such as E-Tran frames.
Objects of reference is using an actual item to give a message, e.g. holding up a CD case to ask for music to be put on.
Paper/paper-based AAC/solutions is any AAC that does not have a battery. Some people used to use the term “low tech”.
Partner assisted scanning (PAS) involves the conversation partner scanning items e.g. letters on an alphabet chart or phrases and symbols, by pointing to and/or saying the names of the items, or reading through a list of options under pragmatic headings, e.g. something’s wrong, I need to, etc. As the partner does the scanning this method does not require the individual to point to any of the items. Partner assisted scanning can be visual, whereby the partner scans the alphabet chart, or by pointing to each item without saying the letters. Auditory scanning involves the partner reading out the letters. Alternatively, visual and auditory scanning can be used together. The method used will depend on the individual’s needs and abilities.
Powered solutions (also known as electronic solutions, and formerly light and high-tech solutions) is technology that makes use of equipment that has a power system. The device usually allows the individual to electronically access speech, picture-graphic, and/or written output. There are a variety of electronic systems. Some are dedicated communication aids; others are PC platforms or tablet devices. Each with different attributes, including voices, shapes, sizes and weights, with capacity to store different amounts of vocabulary.
Receptive language is language that we understand when people are communicating with us. Anything other people use to get a message across to us. It is the opposite of expressive language (see above).
Robust system is AAC that can be used in as many settings as possible. This may need more than one type of AAC, which the user will use at different times (e.g. using a laminated communication board in a swimming pool, but a voice output tablet at other times). It is AAC made suitable for different places and times.
Semantic/schematic is a way to organise words. It will let a user build a sentence on one page of their AAC system but means symbols will be repeated on lots of pages, for example, words such as ‘I’ may come up on nearly every page.
Sign language compared to sign vocabularies – sign languages and sign-vocabularies should be clearly differentiated. British Sign Language (BSL) is a sign language. BSL has its own linguistic structure and semantic concepts. Unaided systems like Makaton and Signalong can be used to describe ‘sign vocabularies’. These are not languages, they are key word ‘sign-vocabularies’ and need everyone to support how they are presented, constructed and taught. Sign vocabularies often support the conversational partner to use sign to converse with the AAC user (aiding comprehension) as much as these sign vocabularies support the AAC user to convey their own key messages.
Supported/scaffolded/co-constructed conversation refers to a number of techniques and strategies that enable effective communication. This could include visual prompts/cues/ramps; starter phrases and word prompts; or checking that use of AAC tools have been understood by the communication partner/s. They all refer to a number of aided and unaided aspects of AAC.
Switch (access) is a button that can be pressed to enable someone with a physical disability to access a wide range of technology, from a light or fan to a voice output communication aid (VOCA) or computer. They come in a variety of sizes and designs and can be accessed using different body parts. In order to control the technology, a switch interface is sometimes required.
Symbol is a (graphic) symbol that may take many forms and acts as a referent for a concept, a word or part of a word. A particular symbol may represent multiple concepts simultaneously, requiring creative interpretation of intended meaning.
Unaided communication (formerly may have been referred to as no-tech solutions) refers to the use of methods involving the user’s body. Includes body movements, facial expressions, gestures, signing, eye-pointing, fixed gaze and vocalisations. Unaided communication is often more efficient and quicker, but relies on the inter-dependence of close communication understanding and shared knowledge of the unaided methods to be effective.
Voice banking is a process by which you create a personalised synthesised voice that should sound more like your existing voice than an ‘off-the-shelf’ voice. This personalised voice can be used to speak out anything that is inputted into an electronic communication aid.
Voice donating is a process through which regional dialects are collected, offering AAC users speech output that more closely resembles their own regional dialect. Currently, this is not automatically available on all devices.
Voice output communication aids (VOCA), also referred to as speech generating devices (SGDs): store speech which can be used to create utterances using individual words or phrases. The speech output may use digitised (pre-recorded) speech, synthesised (artificial) speech or both. Digitised messages are created by recording spoken words directly into the communication aid. Synthesised speech is artificial, computer-generated speech.
Definitions of speech and language diagnoses where AAC may be relevant:
All developmental, lifespan, acquired unless specifically stated (presented alphabetically):
Aphasia – see RCSLT guidance for definition
Aphonia/dysphonia (including laryngectomy)
“Dysphonia refers to disordered sound production at the level of the larynx,” i.e. difficulties with the voice including breath control, pitch and voice quality. (See Cohen et al.) Aphonia is total absence of voice.
Autism – see RCSLT guidance for definition
Cognitive communication impairment
Cognitive communication impairments are problems with communication that have an underlying cause in a cognitive deficit rather than a primary language or speech deficit. They affect:
- attention (selective concentration)
- memory (recall of facts, procedures and past and future events)
- perception (interpretation of sensory information)
- insight and judgment (understanding one’s own limitations and what they mean)
- organisation (arranging ideas in a useful order)
- orientation (knowing where, when and who you are, as well as why you are there)
- language (words for communication)
- processing speed (quick thinking and understanding)
- problem solving (finding solutions to obstacles)
- reasoning (thinking through situations logically)
- executive functioning (making a plan, acting it out, evaluating success and adjusting)
- metacognition (thinking about how you think)
Developmental language disorder – see RCSLT guidance for definition
Dysarthria/anarthria – dysarthria is where you have difficulty speaking because the muscles you use for speech are weak. It can be caused by conditions that damage your brain or nerves and some medicines. Anarthria is being without speech.
Dysfluency (stammer) – see RCSLT guidance for definition.
Dyspraxia/apraxia – a common disorder that affects movement and co-ordination.
Learning disabilities – see RCSLT guidance for definition
Selective mutism (sometimes known as situational mutism) – see RCSLT guidance for definition
Social communication disorder (sometimes known as social communication differences) – see RCSLT guidance for definition
Speech sound disorders – see RCSLT guidance for definition
Contributors
Lead Author
Professor Janice Murray
Supporting Authors
Sinead Barker
Bronagh Blaney
Claire Cardador
Mary Dunningham
Gillian Hazell
Jenny Herd
Catherine Martin
Beth Moulam
Jamie Preece
Katie Radtke
Katherine Small
Emma Sullivan
Helen Whittle
References
Babb, S., Gormley, J., McNaughton, D. and Light, J., (2019). Enhancing independent participation within vocational activities for an adolescent with ASD using AAC video visual scene displays. Journal of Special Education Technology, 34(2), pp.120-132.
Babb, S., McNaughton, D., Light, J. and Caron, J. (2021). “Two friends spending time together”: The impact of video visual scene displays on peer social interaction for adolescents with autism spectrum disorder. Language, Speech, and Hearing Services in Schools, 52(4), pp.1095-1108.
Baker, B.R. (1994). Semantic compaction: An approach to a formal definition. In Proc. 6th Annual European Minspeak Conference (pp.1-5).
Baker, B. and Nyberg, E. (1990). Semantic compaction: A basic technology for artificial intelligence in AAC. In 5th Annual Minspeak Conference (Vol. 32).
Balandin, S. and Johnson, H., 2001. Semantic organisation of adults with cerebral palsy. Advances in Speech Language Pathology, 3(1), pp.1-11.
Balandin, S. and Molka-Danielsen, J. (2015). Teachers’ perceptions of virtual worlds as a medium for social inclusion for adults with intellectual disability. Disability and Rehabilitation, 37(17), pp.1543-1550.
Ball, L.J. and Lasker, J. (2013). Teaching partners to support communication for adults with acquired communication impairment. Perspectives on Augmentative and Alternative Communication, 22(1), pp.4-15.
Batorowicz, B., Stadskleiv, K., Renner, G., Sandberg, A.D. and von Tetzchner, S. (2018). Assessment of aided language comprehension and use in children and adolescents with severe speech and motor impairments. Augmentative and Alternative Communication, 34(1), pp.54-67.
Batorowicz, B., Stadskleiv, K., von Tetzchner, S. and Missiuna, C. (2016). Children who use communication aids instructing peer and adult partners during play-based activity. Augmentative and Alternative Communication, 32(2), pp.105-119.
Bean, A., Harris, K., Kim, H., DiGiovine, C. and Sonntag, A.M. (2023). A scoping review of communication outcomes measures in augmentative and alternative communication. Assistive Technology, 13, pp.1-22.
Beck, A. R., Stoner, J. B. and Dennis, M. L. (2009). An investigation of aided language stimulation: Does it increase AAC use with adults with developmental disabilities and complex communication needs? Augmentative and Alternative Communication, 25(1), pp.42–54.
Berenguer, C., Martínez, E.R., De Stasio, S. and Baixauli, I.(2022). Parents’ perceptions and experiences with their children’s use of augmentative/alternative communication: A systematic review and qualitative meta-synthesis. International Journal of Environmental Research and Public Health, 19(13), p.8091.
Bernal, G., Bonilla, J. and Bellido, C. (1995). Ecological validity and cultural sensitivity for outcome research: Issues for the cultural adaptation and development of psychosocial treatments with Hispanics. Journal of Abnormal Child Psychology, 23, pp.67-82.
Beukelman, D.R., Hux, K., Dietz, A., McKelvey, M. and Weissling, K. (2015). Using visual scene displays as communication support options for people with chronic, severe aphasia: A summary of AAC research and future research directions. Augmentative and Alternative Communication, 31(3), pp.234-245.
Beukelman, D., and Mirenda, P. (2013). Augmentative and alternative communication: Supporting children and adults with complex communication needs (4th ed.). Baltimore, MD: Paul H. Brookes.
Biggs, E.E., Carter, E.W. and Gilson, C.B. (2018). Systematic review of interventions involving aided AAC modeling for children with complex communication needs. American Journal on Intellectual and Developmental Disabilities, 123(5), pp.443-473.
Binger, C. and Light, J. (2007). The effect of aided AAC modeling on the expression of multi-symbol messages by preschoolers who use AAC. Augmentative and Alternative Communication, 23(1), pp.30-43.
Binger, C., Maguire-Marshall, M. and Kent-Walsh, J. (2011). Using aided AAC models, recasts and contrastive targets to teach grammatical morphemes to children who use AAC. Journal of Speech, Language, and Hearing Research, 54(1), pp.160-176.
Binger, C., Kent-Walsh, J., King, M. and Mansfield, L. (2017). Early sentence productions of 3- and 4-year-old children who use augmentative and alternative communication. Journal of Speech, Language, and Hearing Research, 60(7), pp.1930-1945.
Binger, C., Kent-Walsh, J., Harrington, N. and Hollerbach, Q.C. (2020). Tracking early sentence-building progress in graphic symbol communication. Language, Speech and Hearing Services in Schools, 51(2), pp.317-328.
Binger, C., Harrington, N. and Kent-Walsh, J. (2024). Applying a developmental model to preliterate aided language learning. American Journal of Speech-Language Pathology, 33(1), pp.33-50.
Blackstone, S. (1993). Thinking a little harder about communication displays. Augmentative Communication News, 6(1), pp.1-3.
Bloch, S. and Beeke S. (2022). A Better Conversations approach for people living with dysarthria, in Walshe, M. and Miller, N. (eds) Clinical cases in acquired dysarthria, pp 117-127. Routledge
Bloch, S. and Tuomainen, J. (2017). Progressive dysarthria and augmentative and alternative communication in conversation: Establishing the reliability of the Dysarthria-in-Interaction Profile. International Journal of Language and Communication Disorders, 52(1), pp.3-9
Boesch, M.C., Wendt, O., Subramanian, A. and Hsu, N. (2013). Comparative efficacy of the Picture Exchange Communication System (PECS) versus a speech-generating device: Effects on social-communicative skills and speech development. Augmentative and Alternative Communication, 29(3), pp.197-209.
Bondy, A. (2012). The unusual suspects: Myths and misconceptions associated with PECS. The Psychological Record, 62(4), pp. 789-816.
Boster, J.B., McCarthy, J.W., Benigno, J.P., Ottley, J., Spitzley, A.M. and Montgomery, J. (2022). Increasing reciprocal social interactions using collaborative art activities: An intervention for children with complex communication needs and their peers. International Journal of Speech-Language Pathology, 24(2), pp.145-155.
Bradshaw, J. (2013). The use of augmentative and alternative communication apps for the Ipad, Ipod and Iphone: An overview of recent developments. Tizard Learning Disability Review, 18(1), pp.31-37.
Broberg, M., Ferm, U. and Thunberg, G. (2012). Measuring responsive style in parents who use AAC with their children: Development and evaluation of a new instrument. Augmentative and Alternative Communication, 28(4), pp.243-253.
Brock, K., Koul, R., Corwin, M. and Schlosser, R. (2017). A comparison of visual scene and grid displays for people with chronic aphasia: A pilot study to improve communication using AAC. Aphasiology, 31(11), pp.1282-1306.
Broomfield, K., Harrop, D., Judge, S., Jones, G. and Sage, K. (2019). Appraising the quality of tools used to record patient-reported outcomes in users of augmentative and alternative communication (AAC): A systematic review. Quality of Life Research, 28, pp.2669-2683.
Bruno, J. and Trembath, D. (2006). Use of aided language stimulation to improve syntactic performance during a weeklong intervention program. Augmentative and Alternative Communication, 22(4), pp.300-313.
Buchholz, M., Ferm, U. and Holmgren, K. (2019). Digital communication and social media for people with communicative and cognitive disabilities. In Everyday Technologies in Healthcare (pp.193-211). CRC Press.
Buell, S., Bradshaw, J., Bissell, S., Chadwick, D. and Allen, D. (2021). Communication with children with severe or profound intellectual disabilities: A guide for parents. Cerebra Guide.
Burnham, S.P., Finak, P., Henderson, J.T., Gaurav, N., Batorowicz, B., Pinder, S.D. and Davies, T.C. (2023). Models and frameworks for guiding assessment for aided augmentative and alternative communication (AAC): A scoping review. Disability and Rehabilitation: Assistive Technology, pp.1-15.
Carroll, W.R. and Bandura, A. (1985). Role of timing of visual monitoring and motor rehearsal in observational learning of action patterns. Journal of Motor Behavior, 17(3), pp.269-281.
Cave, R. and Bloch, S. (2023). The use of speech recognition technology by people living with amyotrophic lateral sclerosis: A scoping review. Disability and Rehabilitation: Assistive Technology, 18(7), pp.1043-1055.
Cave, R. and Bloch, S. (2021). Voice banking for people living with motor neurone disease: Views and expectations. International Journal of Language and Communication Disorders, 56(1), pp.116-129.
Clarke, M.T., Sargent, J., Cooper, R., Aberbach, G., McLaughlin, L., Panesar, G., Woghiren, A., Griffiths, T., Price, K., Rose, C. and Swettenham, J. (2022). Development and testing of the eye-pointing classification scale for children with cerebral palsy. Disability and Rehabilitation, 44(8), pp.1451-1456.
Clendon, S., Erickson, K., van Rensburg, R.J. and Amm, J. (2014). Shared storybook reading: An authentic context for developing literacy, language, and communication skills. Perspectives on Augmentative and Alternative Communication, 23(4), pp.182-191.
Clendon, S., Paynter, J., Walker, S., Bowen, R. and Westerveld, M.F. (2021). Emergent literacy assessment in children with autism spectrum disorder who have limited verbal communication skills: A tutorial. Language. Speech, and Hearing Services in Schools, 52(1), pp.165-180.
Communication Matters, 2023 https://www.communicationmatters.org.uk/ (including Communication Matters Journal, papers presenting practice based reflections)
Creer, S., Enderby, P., Judge, S. and John, A. (2016). Prevalence of people who could benefit from augmentative and alternative communication (AAC) in the UK: Determining the need. International Journal of Language and Communication Disorders, 51(6), pp.639-653.
Crestani, C.A.M., Clendon, S.A. and Hemsley, B. (2010). Words needed for sharing a story: Implications for vocabulary selection in augmentative and alternative communication. Journal of Intellectual and Developmental Disability, 35(4), pp.268-278.
Dada, S., May, A., Bastable, K., Samuels, A., Tönsing, K., Wilder, J., Casey, M., Ntuli, C. and Reddy, V. (2022). The involvement matrix as a framework for involving youth with severe communication disabilities in developing health education materials. Health Expectations, 25(3), pp.1004-1015.
Dada, S., Van der Walt, C., May, A.A. and Murray, J. (2021). Intelligent assistive technology devices for persons with dementia: A scoping review. Assistive Technology, 25, pp.1-14.
Dahlgren Sandberg, A., Smith, M. and Larsson, M. (2010). An analysis of reading and spelling abilities of children using AAC: Understanding a continuum of competence. Augmentative and Alternative Communication, 26(3), pp.191-202.
Deckers, S.R., Van Zaalen, Y., Van Balkom, H. and Verhoeven, L. (2019). Predictors of receptive and expressive vocabulary development in children with Down syndrome. International Journal of Speech-Language Pathology, 21(1), pp.10-22.
Dietz, A., McKelvey, M. and Beukelman, D.R. (2006). Visual scene displays (VSD): New AAC interfaces for persons with aphasia. Perspectives on Augmentative and Alternative Communication, 15(1), pp.13-17.
Dietz, A., Wallace, S.E. and Weissling, K. (2020). Revisiting the role of augmentative and alternative communication in aphasia rehabilitation. American Journal of Speech-Language Pathology, 29(2), pp.909-913.
Dithole, K.S., Thupayagale-Tshweneagae, G., Akpor, O.A. and Moleki, M.M. (2017). Communication skills intervention: Promoting effective communication between nurses and mechanically ventilated patients. BMC Nursing, 16(1), pp.1-6.
Draffan, E.A., Kadous, A., Idris, A., Banes, D., Zeinoun, N., Wald, M. and Halabi, N. (2015). A participatory research approach to develop an Arabic symbol dictionary. In Assistive Technology (pp.796-804). IOS Press.
Drager, K.D., Light, J., Currall, J., Muttiah, N., Smith, V., Kreis, D., Nilam-Hall, A., Parratt, D., Schuessler, K., Shermetta, K. and Wiscount, J. (2019). AAC technologies with visual scene displays and “just in time” programming and symbolic communication turns expressed by students with severe disability. Journal of Intellectual and Developmental Disability, 44(3), pp.321-336.
Dooley, J., Bailey, C. and McCabe, R. (2015). Communication in healthcare interactions in dementia: A systematic review of observational studies. International Psychogeriatrics, 27(8), pp.1277-1300.
Dooley, S. and Walshe, M. (2019). Assessing cognitive communication skills in dementia: A scoping review. International Journal of Language and Communication Disorders, 54(5), pp.729-741.
Douglas, N.F., Feuerstein, J.L., Oshita, J.Y., Schliep, M.E. and Danowski, M.L. (2022). Implementation science research in communication sciences and disorders: A scoping review. American Journal of Speech-Language Pathology, 31(3), pp.1054-1083.
Douglas, N.F., Archer, B., Azios, J.H., Strong, K.A., Simmons-Mackie, N. and Worrall, L. (2023). A scoping review of friendship intervention for older adults: Lessons for designing intervention for people with aphasia. Disability and Rehabilitation, 45(18), pp.3012-3031.
Dunér, A., Bångsbo, A. and Olsson, T. M. (2023). Talking Mats as a decision aid to promote involvement in choice and decision-making around home care services for older people with mild to moderate dementia: Study protocol for a randomized controlled trial. BMC Geriatrics, 23(1).
Elmquist, M., Simacek, J., Dimian, A.F. and Reichle, J.( 2019). Impact of aided AAC interventions on speech comprehension of children with neurodevelopmental disabilities: A critically appraised topic. Evidence-based Communication Assessment and Intervention, 13(1-2), pp.67-84.
Elsahar, Y., Hu, S., Bouazza-Marouf, K., Kerr, D. and Mansor, A. (2019). Augmentative and alternative communication (AAC) advances: A review of configurations for individuals with a speech disability. Sensors, 19(8), p.1911.
Emms, L. and Gardner, H. (2010). Study of two graphic symbol-teaching methods for individuals with physical disabilities and alearning difficulties. Child Language Teaching and Therapy, 26(1), pp.5-22.
Enderby, P., Judge, S., Creer, S. and John, A.(2013). Examining the need for and provision of AAC methods in the UK. Advances in Clinical Neuroscience and Rehabilitation, 13, pp.20-23.
Enderby, P. (2014). Introducing the therapy outcome measure for AAC services in the context of a review of other measures. Disability and Rehabilitation: Assistive Technology, 9(1), pp.33-40.
Erickson, K.A., 2017. Comprehensive literacy instruction, interprofessional collaborative practice, and students with severe disabilities. American Journal of Speech-Language Pathology, 26(2), pp.193-205.
Erickson, K.A. and Koppenhaver, D.A.(2020). Comprehensive literacy for all: Teaching students with significant disabilities to read and write. Brookes Publishing Company. PO Box 10624, Baltimore, MD 21285.
Ericsson, K.A., Krampe, R.T. and Tesch-Römer, C. (1993). The role of deliberate practice in the acquisition of expert performance. Psychological Review, 100(3), p.363.
Fäldt, A., Fabian, H., Thunberg, G. and Lucas, S. (2020). “All of a sudden we noticed a difference at home too”: Parents’ perception of a parent-focused early communication and AAC intervention for toddlers. Augmentative and Alternative Communication, 36(3), pp.143-154.
Fjeldvang, R.T., Nordaas, M.G., von Tetzchner, S. and Stadskleiv, K. (2023). Measuring impact of augmentative and alternative communication interventions: Adapting the family impact of assistive technology scale for augmentative and alternative communication (FIATS-AAC-No) for use in Norway. Augmentative and Alternative Communication, 39(3) pp.1-11.
Friedman, M.G., Beckwith, R.M. and Conroy, J.W. (2016). Effective strategies for supporting individuals with complex needs in leadership roles. Inclusion, 4(3), pp.170-182.
Ganz, J.B., Goodwyn, F.D., Boles, M.M., Hong, E.R., Rispoli, M.J., Lund, E.M. and Kite, E. (2013). Impacts of a PECS instructional coaching intervention on practitioners and children with autism. Augmentative and Alternative Communication, 29(3), pp.210-221.
Gevarter, C., Groll, M. and Stone, E. (2020). Dynamic assessment of augmentative and alternative communication application grid formats and communicative targets for children with autism spectrum disorder. Augmentative and Alternative Communication, 36(4), pp.226-237.
Giles, H., Coupland, N. and Coupland, I.U.S.T.I.N.E. (1991). 1. Accommodation theory: Communication, context and consequence. Contexts of Accommodation: Developments in Applied Sociolinguistics, pp1-68.
Glennen, S. and Decoste, D. (1998). Handbook of AAC. New York: Cengage Learning.
Goldbart, J. and Marshall, J. (2004). “Pushes and pulls” on the parents of children who use AAC. Augmentative and Alternative Communication, 20(4), pp.194-208.
Goossens’, C. (1989). Aided communication intervention before assessment: A case study of a child with cerebral palsy. Augmentative and Alternative Communication, 5(1), pp.14-26.
Goossens’ C., Crain S., Elder P. (1992). Engineering the preschool environment for interactive, symbolic communication. Southeast Augmentative Communication Conference Publications, Birmingham, AL.
Griffiths, T., Clarke, M.T. and Swettenham, J. (2023). The ability of typically developing 2–3-year-olds to infer the control mechanism for eye-gaze technology and the impact of causal language instruction. Disability and Rehabilitation: Assistive Technology, pp.1-8.
Gross, J. (2010). Augmentative and alternative communication: A report on provision for children and young people in England. Office of the Communication Champion.
Grove, N. and Launonen, K. (2019). Manual sign acquisition in children with developmental disabilities. Nova Science Publishers.
Hanley, E., Martin, A.M., Dalton, C. and Lehane, E. (2023). Communication partners experiences of communicating with adults with severe/profound intellectual disability through augmentative and alternative communication: A mixed methods systematic review. Journal of Intellectual Disabilities, 27(4), pp.1107-1134.
Harding, C., Lindsay, G., O’Brien, A., Dipper, L. and Wright, J. (2011). Implementing AAC with children with profound and multiple learning disabilities: A study in rationale underpinning intervention. Journal of Research in Special Educational Needs, 11(2), pp.120-129.
Harrison, R.A., Bradshaw, J., Forrester‐Jones, R., McCarthy, M. and Smith, S. (2021). Social networks and people with intellectual disabilities: A systematic review. Journal of Applied Research in Intellectual Disabilities, 34(4), pp.973-992.
Hayes, L.E. and Traughber, M.C. (2021). Improving facilitation of student communication through observational feedback within a partner instruction model. Language, Speech, and Hearing Services in Schools, 52(2), pp.542-553.
Hemsley, B., Dann, S., Palmer, S., Allan, M. and Balandin, S. (2015). “We definitely need an audience”: Experiences of Twitter, Twitter networks and tweet content in adults with severe communication disabilities who use augmentative and alternative communication (AAC). Disability and Rehabilitation, 37(17), pp.1531-1542.
Hill, K. (2006). Augmentative and alternative communication (AAC) research and development: The challenge of evidence-based practice. International Journal of Computer Processing of Oriental Languages, 19(4), pp.249-262.
Huang, L., Chen, S.H.K., Xu, S., Wang, Y., Jin, X., Wan, P., Sun, J., Tao, J., Zhang, S., Zhang, G. and Shan, C. (2021). Augmentative and alternative communication intervention for in-patient individuals with post-stroke aphasia: Study protocol of a parallel-group, pragmatic randomized controlled trial. Trials, 22(1), pp.1-9.
Hutchinson, N. and Bodicoat, A.(2015). The effectiveness of intensive interaction, A systematic literature review. Journal of Applied Research in Intellectual Disabilities, 28(6), pp.437-454.
Hynan, A., Murray, J. and Goldbart, J. (2014). “Happy and excited”: Perceptions of using digital technology and social media by young people who use augmentative and alternative communication. Child Language Teaching and Therapy, 30(2), pp.175-186.
Iacono, T., Bould, E., Beadle‐Brown, J. and Bigby, C., 2019. An exploration of communication within active support for adults with high and low support needs. Journal of Applied Research in Intellectual Disabilities, 32(1), pp.61-70.
International Society for Augmentative and Alternative Communication. (2014). Isaac Position Statement on Facilitated Communication. International Society for Augmentative and Alternative Communication. Augmentative and Alternative Communication, 30(4), pp. 357–8. doi: 10.3109/07434618.2014.971492
James, I. A. and Gibbons, L. (2019). Communication skills for effective dementia care: a practical guide to communication and interaction training. London, UK: Jessica Kingsley.
Judge, S., Enderby, P., Creer, S. and John, A. (2017). Provision of powered communication aids in the United Kingdom. Augmentative and Alternative Communication, 33(3), pp.181-187.
Judge, S., Murray, J., Lynch, Y., Meredith, S., Moulam, L., Randall, N., Whittle, H. and Goldbart, J. (2023). Attributes of communication aids as described by those supporting children and young people with AAC. International Journal of Language and Communication Disorders, 58(3), pp.910-928.
Karlsson, P., Griffiths, T., Clarke, M.T., Monbaliu, E., Himmelmann, K., Bekteshi, S., Allsop, A., Pereksles, R., Galea, C. and Wallen, M. (2021). Stakeholder consensus for decision making in eye-gaze control technology for children, adolescents and adults with cerebral palsy service provision: Findings from a Delphi study. BMC Neurology, 21(1), pp.1-24.
Kent-Walsh, J., Murza, K.A., Malani, M.D. and Binger, C. (2015). Effects of communication partner instruction on the communication of individuals using AAC: A meta-analysis. Augmentative and Alternative Communication, 31(4), pp.271-284.
Kent-Walsh, J. and Binger, C.(2018). Methodological advances, opportunities and challenges in AAC research. Augmentative and Alternative Communication, 34(2), pp.93-103.
Killick, J. and Craig, C. (2012) Creativity and communication in persons with dementia: A practical guide. London: Jessica Kingsley.
Koudys, J., Perry, A. and McFee, K. (2021). Picture Exchange Communication System® (pecs®) use in a community setting: A preliminary investigation. Journal of Developmental and Physical Disabilities, 34(5), pp. 829–852.
Lacey, E.A., Ogletree, B.T., Rice, T. and Rose, A. (2017). Milieu training for adults with severe intellectual disability: A clinical illustration. Communication Disorders Quarterly, 38(3), pp.179-184.
Laher, Z. and Dada, S. (2023). The effect of aided language stimulation on the acquisition of receptive vocabulary in children with complex communication needs and severe intellectual disability: A comparison of two dosages. Augmentative and Alternative Communication, 39(2), pp.96-109.
Light, J., Wilkinson, K.M., Thiessen, A., Beukelman, D.R. and Fager, S.K. (2019). Designing effective AAC displays for individuals with developmental or acquired disabilities: State of the science and future research directions. Augmentative and Alternative Communication, 35(1), pp.42-55.
Light, J. (1989). Toward a definition of communicative competence for individuals using augmentative and alternative communication systems. Augmentative and Alternative Communication, 5(2), pp.137-144.
Light, J. and McNaughton, D. (2012). The changing face of augmentative and alternative communication: Past, present, and future challenges. Augmentative and Alternative Communication, 28(4), pp.197-204.
Light, J. and McNaughton, D. (2015). Designing AAC research and intervention to improve outcomes for individuals with complex communication needs. Augmentative and Alternative Communication, 31(2), pp.85-96.
Light, J., McNaughton, D. and Caron, J. (2019). New and emerging AAC technology supports for children with complex communication needs and their communication partners: State of the science and future research directions. Augmentative and Alternative Communication, 35(1), pp.26-41.
Light, J., Wilkinson, K.M., Thiessen, A., Beukelman, D.R. and Fager, S.K. (2019). Designing effective AAC displays for individuals with developmental or acquired disabilities: State of the science and future research directions. Augmentative and Alternative Communication, 35(1), pp.42-55.
Lynch, Y., McCleary, M. and Smith, M. (2018). Instructional strategies used in direct AAC interventions with children to support graphic symbol learning: A systematic review. Child Language Teaching and Therapy, 34(1), pp.23-36.
Lynch, Y., Murray, J., Moulam, L., Meredith, S., Goldbart, J., Smith, M., Batorowicz, B., Randall, N. and Judge, S. (2019). Decision-making in communication aid recommendations in the UK: Cultural and contextual influencers. Augmentative and Alternative Communication, 35(3), pp.180-192.
Lynch, Y. and Murray, J. (2023). The I-ASC Explanatory Model as a support for AAC assessment planning: A case report (Ch 2) In Smith, M.M. (Ed.). (2023). Clinical cases in augmentative and alternative communication (1st ed.). Routledge.
May, A., Dada, S. and Murray, J. (2023). Implementing AAC for a person with dementia (Ch 12) In Smith, M.M. (Ed.). (2023). Clinical cases in augmentative and alternative communication (1st ed.). Routledge.
Millar, S. with Aitken, S. (2003). Personal communication passports: Guidelines for good practice. Edinburgh: CALL Centre.
Midtlin, H.S., Næss, K.A.B., Taxt, T. and Karlsen, A.V. (2015). What communication strategies do AAC users want their communication partners to use? A preliminary study. Disability and Rehabilitation, 37(14), pp.1260-1267.
Mood, D., Sheldon, R., Tabangin, M., Wiley, S. and Meinzen-Derr, J. (2022). Technology assisted language intervention (TALI) for children who are deaf/hard of hearing: Promising impact on pragmatic skills. Deafness and Education International, 24(4), pp.334-355.
Moorcroft, A., Scarinci, N. and Meyer, C. (2018). A systematic review of the barriers and facilitators to the provision and use of low-tech and unaided AAC systems for people with complex communication needs and their families. Disability and Rehabilitation: Assistive Technology, 14(7), pp.710-731
Moorcroft, A., Scarinci, N. and Meyer, C. (2019). Speech pathologist perspectives on the acceptance versus rejection or abandonment of AAC systems for children with complex communication needs. Augmentative and Alternative Communication, 35(3), pp.193-204.
Murray, J. and Goldbart, J. (2011. Emergence of working memory in children using aided communication. Journal of Assistive Technologies, 5(4), pp.214-232.
Murray, J. and Goldbart, J. (2009). Cognitive and language acquisition in typical and aided language learning: A review of recent evidence from an aided communication perspective. Child Language Teaching and Therapy, 25(1), pp.31-58.
Murray, J., Bell, H., and Goldbart, J. (2016). Operational demands and representational forms. In M. M. Smith and J. Murray (Eds.), The silent partner? Language, interaction and aided communication (pp.35-64). Guildford, UK, Surrey: J&R Press.
Murray, J., Lynch, Y., Meredith, S., Moulam, L., Goldbart, J., Smith, M., Randall, N. and Judge, S. (2019). Professionals’ decision making in recommending communication aids in the UK: Competing considerations. Augmentative and Alternative Communication, 35(3), pp.167-179.
Murray, J., Dada, S. and May, A. (2022). Dementia and augmentative and alternative communication: Supporting conversations. Karger Publishers Ltd, Freiburg: Germany
Murphy, J. and Oliver, T. (2013). The use of Talking Mats to support people with dementia and their carers to make decisions together. Health and Social Care in the Community, 21(2), pp.171-180.
Murphy, J. and Boa, S. (2013). A critical appraisal of existing methods of measuring outcomes in relation to augmentative and alternative communication. NHS Education for Scotland.
Naguib Bedwani, M.A., Bruck, S. and Costley, D. (2015). Augmentative and alternative communication for children with autism spectrum disorder: An evidence-based evaluation of the Language Acquisition through Motor Planning (LAMP) programme. Cogent Education, 2(1), p.1045807.
Neuvonen, K.A., Launonen, K., Smith, M.M., Stadskleiv, K. and von Tetzchner, S. (2022). Strategies in conveying information about unshared events using aided communication. Child Language Teaching and Therapy, 38(1), pp.78-94.
NHS Education or Scotland. Informing and Profiling AAC Knowledge and Skills (IPAACKs): link ipaacks.pdf (aacscotland.org.uk)
NICE, 2012. Guideline CG142 Autism spectrum disorder in adults: diagnosis and management.
Norrie, C. S., Waller, A. and Hannah, E. F. S. (2021). Establishing Context: AAC Device adoption and support in a special-education setting. ACM Transactions on Computer-Human Interaction (TOCHI), 28(2), pp.1-30.
Ogletree, B.T., Bartholomew, P., Kirksey, M.L., Guenigsman, A., Hambrecht, G., Price, J. and Wofford, M.C. (2016). Communication training supporting an AAC user with severe intellectual disability: Application of the communication partner instruction model. Journal of Developmental and Physical Disabilities, 28, pp.135-152.
Ogletree, B.T., Wofford, M.C. and Barton-Hulsey, A. (2022). Practical approaches and socially valid assessment considerations for learners with emergent communication and severe intellectual disability. Advances in Neurodevelopmental Disorders, 6(4), pp.426-441.
Omahen, D.A. (2009). The 10 000-hour rule and residency training. Canadian Medical Association Journal, 180(12), pp.1272-1272.
O’Neill, T., Wilkinson, K. M. and Light, J. (2019). Preliminary investigation of visual attention to complex AAC visual scene displays in individuals with and without developmental disabilities. Augmentative and Alternative Communication, 35(3), pp.240-250.
Pampoulou, E. and Fuller, D. R. (2021). Introduction of a new AAC symbol classification system: The multidimensional quaternary symbol continuum. Journal of Enabling Technologies, 15(4), pp.252-267.
Pampoulou, E. and Fuller, D. R. (2020). Exploring AAC graphic symbol choices: A preliminary study. Journal of Enabling Technologies, 14(3), pp.171-185.
Pert, S. (2022). Working with children experiencing speech and language disorders in a bilingual context: A home language approach. Taylor & Francis.
Pilesjö, M.S. and Norén, N. (2019). Facilitators’ use of a communication device following children’s aided turns in everyday interaction. Journal of Interactional Research in Communication Disorders, 10(1), pp.67-98.
Porter, G. and Burkhart, L. (2010). Limitations with using a representational hierarchy approach for language learning. https://lindaburkhart.com/wp-content/uploads/2016/07/representational_hierarchy_draft.pdf
Porter, G. and Cafiero, J.M. (2009). Pragmatic organization dynamic display (PODD) communication books: A promising practice for individuals with autism spectrum disorders. Perspectives on Augmentative and Alternative Communication, 18(4), pp.121-129.
Porter, G. and Cameron, M. (2007). CHAT-Now manual: Children’s aided language tools. Melbourne, Australia: Scope Victoria.
Quinn, E.D., Cook, A., Wiedrick, J. and Rowland, C. (2021). An initial investigation into the feasibility of the communication matrix professional development program for educational professionals working with students with complex communication needs. Language, Speech, and Hearing Services in Schools, 52(4), pp.1080-1094.
Raghavendra, P., Bornman, J., Granlund, M. and Björck-Åkesson, E. (2007). The World Health Organization’s International Classification of Functioning, Disability and Health: Implications for clinical and research practice in the field of augmentative and alternative communication. Augmentative and Alternative Communication, 23(4), pp.349-361.
Raghavendra, P. and Swift, M. (2019). Special issue on critically appraised topics in communication disorders: Research evidence for use in clinical practice. Evidence-based Communication Assessment and Intervention, 13(1-2), pp.1-2.
Rezayi, S. (2022). The effectiveness of an Intensive Interaction intervention program based on sensory approach on challenging behaviors of children with autism disorder. Journal of Exceptional Children, 22(3), pp.111-122.
Robinson, H. (2022). The four Ps of AAC.
Romski, M. and Sevcik, R.A. (2005). Augmentative communication and early intervention: Myths and realities. Infants and Young Children, 18(3), pp.174-185.
Rowland, C., Fried-Oken, M., Bowser, G., Granlund, M., Lollar, D., Phelps, R., Simeonsson, R.J. and Steiner, S.A. (2016). The Communication Supports Inventory-Children and Youth (CSI-CY), a new instrument based on the ICF-CY. Disability and Rehabilitation, 38(19), pp.1909-1917.
Rush, K. S., Mortenson, B. P. and Birch, S. E. (2020). The inadvertent effects of PECS on vocal responding of children with autism spectrum disorder. Advances in Neurodevelopmental Disorders: Multidisciplinary Research and Practice Across the Lifespan, 4(3), pp.308-318.
Sadiku, L., Small. and Martin, S. (2022). Augmentative and alternative communication (Ch 8) IN Pert, S. (2022). Working with children experiencing speech and language disorders in a bilingual context: A home language approach. Taylor & Francis.
Schlosser, R. W. (2003). The efficacy of augmentative and alternative communication: towards evidence based practice. London: Academic Press.
Schlosser, R.W., Wendt, O., Angermeier, K. and Shetty, M. (2005). Searching for evidence in augmentative and alternative communication: Navigating a scattered literature. Augmentative and Alternative Communication, 21(4), 233-255.
Sellwood, D., Raghavendra, P. and Walker, R. (2022). Facilitators and barriers to developing romantic and sexual relationships: Lived experiences of people with complex communication needs. Augmentative and Alternative Communication, 38(1), pp.1-14.
Semel, E., Wiig, E., Secord, W. and Sample, N. (2004). Test review: Clinical evaluation of language fundamentals-4 (CELF-4). San Antonio, TX: Psychological Corporation.
Sennott, S.C., Light, J.C. and McNaughton, D. (2016). AAC modeling intervention research review. Research and Practice for Persons with Severe Disabilities, 41(2), pp.101-115.
Sherlock, C. (2011). Becoming ready to use a voice output communication aid. Journal of Assistive Technologies, 5(4), pp. 233-241.
Shire, S.Y. and Jones, N. (2015). Communication partners supporting children with complex communication needs who use AAC: A systematic review. Communication Disorders Quarterly, 37(1), pp.3-15.
Smith, A. L. and Hustad, K. C. (2015). AAC and early intervention for children with cerebral palsy: Parent perceptions and child risk factors. Augmentative and Alternative Communication, 31(4), pp. 336-50.
Smith, M.M. (2015). Language development of individuals who require aided communication: Reflections on state of the science and future research directions. Augmentative and Alternative Communication, 31(3), pp.215-233.
Smith, M.M. (Ed.). (2023). Clinical cases in augmentative and alternative communication (1st ed.). Routledge. https://doi.org/10.4324/9781003106739
Smith, M.M. and Murray, J. (2011). Parachute without a ripcord: The skydive of communication interaction. Augmentative and Alternative Communication, 27(4), pp.292-303.
Smith, M.M. and Murray, J. eds. (2016). The silent partner? Language, interaction and aided communication. J&R Press Limited.
Soto, G., Yu, B. and Kelso, J. (2008). Effectiveness of multifaceted narrative intervention on the stories told by a 12-year-old girl who uses AAC. Augmentative and Alternative Communication, 24(1), pp.76-87.
Soto, G. and Zangari, C., 2009. Practically speaking. Language, literacy and academic development for students with AAC needs. Brookes Pub Co: Baltimore, USA
Stadskleiv, K., Batorowicz, B., Sandberg, A.D., Launonen, K., Murray, J., Neuvonen, K., Oxley, J., Renner, G., Smith, M.M., Soto, G. and van Balkom, H. (2022). Aided communication, mind understanding and co-construction of meaning. Developmental Neurorehabilitation, 25(8), pp.518-530.
Stadskleiv, K., Jahnsen, R., Andersen, G.L. and von Tetzchner, S. (2017). Executive functioning in children aged 6–18 years with cerebral palsy. Journal of Developmental and Physical Disabilities, 29, pp.663-681.
Stadskleiv, K., Van Walsem, M.R., Andersen, G.L., Bergqvist, L., Bøttcher, L., Christensen, K., Heyerdahl, D., Hollung, S.J., Høye, H., Jahnsen, R. and Klevberg, G.L. (2021). Systematic monitoring of cognition for adults with cerebral palsy: The rationale behind the development of the CP Cog-Adult Follow-Up Protocol. Frontiers in Neurology, 12, p.710440.
Starble, A., Hutchins, T., Favro, M.A., Prelock, P. and Bitner, B. (2005). Family-centered intervention and satisfaction with AAC device training. Communication Disorders Quarterly, 27(1), pp.47-54.
Stendal, K., Balandin, S. and Molka-Danielsen, J. (2011). Virtual worlds: A new opportunity for people with lifelong disability? Journal of Intellectual and Developmental Disability, 36(1), pp.80-83.
Stipinovich, A.M., Tönsing, K. and Dada, S. (2023). Communication strategies to support decision‐making by persons with aphasia: A scoping review. International Journal of Language and Communication Disorders, 58(6), pp.1955-1976.
Stuart, S. and Ritthaler, C. (2008). Case studies of intermediate steps/between AAC evaluations and implementation. Perspectives on Augmentative and Alternative Communication, 17(4), pp.150-155.
Sutton, A., Trudeau, N., Morford, J.P., Smith, M.M. and Mascolo, M.È. (2022). Expressive and receptive performance with graphic symbol sentences by individuals who use aided communication. Augmentative and Alternative Communication, 38(3), pp.135-147.
Swinburn, K., Porter, G. and Howard, D. (2004). Comprehensive aphasia test. APA PsycTests. https://doi.org/10.1037/t13733-000
Thiessen, A. and Beukelman, D. (2013). Training communication partners of adults who rely on AAC: Co-construction of meaning. Perspectives on Augmentative and Alternative Communication, 22(1), pp.16-20.
Thiessen, A. and Brown, J. (2021). Personalization of restorative and compensatory treatments for people with aphasia: A review of the evidence. Topics in Language Disorders, 41(3), pp.269-281.
Thistle, J.J. and Wilkinson, K.M. (2013). Working memory demands of aided augmentative and alternative communication for individuals with developmental disabilities. Augmentative and Alternative Communication, 29(3), pp.235-245.
Thistle, J.J. and Wilkinson, K.M. (2015). Building evidence-based practice in AAC display design for young children: Current practices and future directions. Augmentative and Alternative Communication, 31(2), pp.124-136.
Thistle, J. J. and Wilkinson, K. (2017). Effects of background color and symbol arrangement cues on construction of multi-symbol messages by young children without disabilities: Implications for aided AAC design. Augmentative and Alternative Communication, 33(3), pp.160169.
Thistle, J.J. and Wilkinson, K.M. (2021). Speech-Language pathologists’ decisions when designing an aided AAC display for a compilation case study of a beginning communicator. Disability and Rehabilitation: Assistive Technology, 16(8), pp.871-879.
Tönsing, K.M. and Dada, S. (2023). Learning graphic symbols in two languages: Effects of monolingual teaching. International Journal of Speech-Language Pathology, 25(2), pp.281-291.
Tönsing, K.M. and Soto, G. (2020). Multilingualism and augmentative and alternative communication: Examining language ideology and resulting practices. Augmentative and Alternative Communication, 36(3), pp.190-201.
Trnka, K., McCaw, J., Yarrington, D., McCoy, K.F. and Pennington, C. (2009) User interaction with word prediction: The effects of prediction quality (preprint). ACM Transactions on Accessible Computing 1(3), pp1-34.
Trnka, K. and McCoy, K.F. (2008). Evaluating word prediction: Framing keystroke savings. In Proceedings of acl-08: Hlt, short papers, pp.261-264.
Vaillant, E., Oostrom, K.J., Beckerman, H., Vermeulen, R.J., Buizer, A.I. and Geytenbeek, J.J. (2024). Developmental trajectories of spoken language comprehension and functional communication in children with cerebral palsy: A prospective cohort study. Developmental Medicine and Child Neurology, 66(1), pp.95-105.
Valiquette, C., Gérin-Lajoie, A.-M. and Sutton, A. (2006). A visual graphic tool to support the production of simple sentence structures in a student with learning disability. Child Language Teaching and Therapy, 22(2), pp.219-240.
Volkmer, A., Walton, H., Swinburn, K., Spector, A., Warren, J.D. and Beeke, S. (2023). Results from a randomised controlled pilot study of the Better Conversations with Primary Progressive Aphasia (BCPPA) communication partner training program for people with PPA and their communication partners. Pilot and Feasibility Studies, 9(1), p.87.
von Tetzchner, S. (2015) The semiotics of aided language development. Cognitive Development, 36, pp.180-190.
von Tetzchner, S. (2018). Introduction to the special issue on aided language processes, development, and use: An international perspective. Augmentative and Alternative Communication, 34(1), pp.1-15.
von Tetzchner, S., Martinsen, H. and Stadskleiv, K. (2024). Augmentative and alternative communication for children, adolescents and adults with developmental disabilities. Abingdon, UK: Routledge.
von Tetzchner, S. and Murray, J. (eds). (2022). Becoming an aided communicator (BAC): Theory, methods, findings and practical implications. Proceedings of Communication Matters’ Study Day, Leeds, 21 June 21 2022. Leeds, UK: Communication Matters.
Wallace, S.E. and Hux, K. (2014). Effect of two layouts on high technology AAC navigation and content location by people with aphasia. Disability and Rehabilitation: Assistive Technology, 9(2), pp.173-182.
Waller, A. and Newell, A.F. (1997). Towards a narrative‐based augmentative communication system. International Journal of Language and Communication Disorders, 32(S3), pp.289-306.
Waller, A. (2019). Telling tales: Unlocking the potential of AAC technologies. International Journal of Language and Communication Disorders, 54(2), pp.159-169.
Walker, N. (2021) Neuroqueer heresies: Notes on the neurodiversity paradigm, autistic empowerment, and postnormal possibilities. Fort Worth, TX: Autonomous Press.
Wang, H., Fu, T., Du, Y., Gao, W., Huang, K., Liu, Z., Chandak, P., Liu, S., Van Katwyk, P., Deac, A. and Anandkumar, A.(2023). Scientific discovery in the age of artificial intelligence. Nature, 620(7972), pp.47-60.
Ware, J., Buell, S., Chadwick, D.D., Bradshaw, J. and Goldbart, J. (2024). A systematic review of research on staff training as an intervention to develop communication in children and adults with profound intellectual and multiple disabilities. Journal of Applied Research in Intellectual Disabilities, 37(2), p.e13201.
Webb, E.J., Meads, D., Lynch, Y., Judge, S., Randall, N., Goldbart, J., Meredith, S., Moulam, L., Hess, S. and Murray, J. (2021). Attribute selection for a discrete choice experiment incorporating a best-worst scaling survey. Value in Health, 24(4), pp.575-584.
Webb, E.J.D., Meads, D., Lynch, Y., Randall, N., Judge, S., Goldbart, J., Meredith, S., Moulam, L., Hess, S. and Murray, J. (2023). Something for everybody? Assessing the suitability of AAC systems for children using stated preference methods, Augmentative and Alternative Communication, 39(3), pp.157-169.
Wilkinson, K. M., Light, J. and Drager, K. (2012). Considerations for the composition of visual scene displays: Potential contributions of information from visual and cognitive sciences. Augmentative and Alternative Communication, 28(3), pp.137-147.
Witkowski, D. and Baker, B. (2012). Addressing the content vocabulary with core: Theory and practice for nonliterate or emerging literate students. Perspectives on Augmentative and Alternative Communication, 21(3), pp.74-81.
World Health Organization, 2007. International Classification of Functioning, Disability, and Health: Children and Youth Version: ICF-CY. World Health Organization.
Yung-Chin T., Chun-Chieh S. and Tian-Syung L. (2019). Development of a reminiscence therapy system for the elderly using the integration of virtual reality and augmented reality. Sustainability 11(17), pp. 4792. doi: 10.3390/su11174792.
Zinkevich, A., Uthoff, S.A.K., Wirtz, M.A., Boenisch, J., Sachse, S.K., Bernasconi, T., Feldhaus, M. and Ansmann, L. (2022). Burden of informal caregivers of people without natural speech: A mixed-methods intervention study. BMC Health Services Research, 22(1), pp.1-14.

 Download as PDF
Download as PDF

